PATIENT EDUCATION MATERIAL
 Contributions from
Contributions from
SIG and IRA team with special mention toDr. Nilesh NolkhaWockhardt Hospital, Mumbai
Dr. Shashank M AkerkarMumbai Arthritis Clinic, Mumbai
Dr. C BalajiSri Ramachandra Medical College, Chennai
Dr. Avinash JainSGPGI, Lucknow
Dr. Padmanabha ShenoyCARE, Cochin, Kerala
Disease Specific information
ANKYLOSING SPONDYLITIS (AS) - FAQs
What is Ankylosing spondylitis?
It is a type of spondyloarthritis, an autoimmune disease which targets the spine predominantly.
Ankylos- stiffening of joint
Spondlyo – vertebrae
What causes Ankylosing spondylitis?
Exact cause is unknown. Most autoimmune disease have genetic risk factors and environmental triggers which dysregulate immune system. The immune system starts attacking the joints & other structures. In AS, it attacks the sacroiliac joints, joints of the vertebrae, hip & occasionally the other joints. It may also attack other structures including the eyes.
In what way is Ankylosing spondylitis different from other arthritis like Rheumatoid arthritis?
In Rheumatoid arthritis, inflammation of joints is the hallmark whereas in AS the sites where ligaments and tendons attach to bones called entheses are inflamed. Rheumatoid arthritis predominantly affects the hand & feet joints as well as large joints like the knee, ankle, shoulder. Ankylosing spondylitis mainly affects the sacroiliac joints (located beneath the buttocks), vertebral joints & hips, knee & ankle.
Who gets Ankylosing Spondylitis?
AS usually begins in adolescents/young adults. It presents usually before 45 years of age. Men 2-3 times more likely to develop AS than women. Family members of patients with AS are also at a higher risk.
What is the most common symptom of Ankylosing spondylitis?
Main symptom of AS is low back pain. Back pain of ankylosing spondylitis usually is severe at rest and gets better with activity. It is more severe in the nights and is associated with a stiff back early in the morning for atleast more than 30 minutes.
Can Ankylosing spondylitis also cause pains in limbs ?
AS can also cause joint pains usually in the lower limbs. Heel pain, sole pain are also common.
How is Ankylosing Spondylitis diagnosed ?
Rheumatologist asseses your medical history , examines the musculoskeletal system and based on the clinical scenario orders for imaging and blood tests. Xray of sacroiliac joint ± spine or MRI may be ordered to make a diagnosis. HLA B27 genetic testing may also be ordered as a part of work up.
If I have HLA B27 positivity, does that mean I have AS ?
Not always. Some people have the HLA-B27 gene but do not develop AS. This test has to be interpreted by your Rheumatologist in conjunction with the clinical scenario and imaging evidence.
Can the HLA B27 test be negative in ankylosing spondylitis?
Yes. HLA B27 is positive in majority of the patients. However there are other genes that can cause AS & HLA B 27 is need not always be positive in a person suffering from AS. This also means that AS can be diagnosed without the HLA- B 27 test.
How does Ankylosing spondylitis progress?
Over a period of time with persistent inflammation, calcium gets deposited on ligaments of the spine. The vertebral joints fuse & become stiff. This leads to difficulty in bending, turning the neck.
How do Xray/ MRI help diagnosis of ankylosing spondylitis?
Xrays pick up the calcification of spinal ligaments & fusion of the sacroiliac joints. This helps diagnosis of AS. However calcification of the ligaments happens after years & hence X-rays can miss the diagnosis of AS in early stages. MRI picks up the inflammation (swelling) in the sacroiliac joints & help early diagnosis of AS.
Can Ankylosing spondylitis be cured ?
There is no cure for AS. But early treatment relieves symptoms and prevents progression of disease.
How is Ankylosing spondylitis treated?
The first line of treatment are the NSAIDs / pain killers like indomethacin, diclofenac, aceclofenac etc. No NSAID is superior to another. These drugs give relief from pain for most patients.
For joint and tendon related pains local injections of steroids (localized joint pain, tendon sheaths) or oral steroids (multiple joint pains) are effective. If there is no response to the above treatment, disease modifying antirheumatic drugs (DMARDs) such as sulfasalazine, methotrexate, leflunomide may be useful.
STEROIDS AND DMARDS HAVE NO PROVEN ROLE IN RELIEVING SPINAL SYMPTOMS AND HALTING THE DISEASE PROGRESSION IN THE SPINE.
Biologics like TNF alpha blockers are the most effective drugs available in treating the spinal and peripheral joint symptoms. Examples of TNF alpha blockers available in our country are infliximab (administered as Intravenous infusion), etanercept, adalimumab, golimumab (administered under the skin).
However TNF alpha blockers are expensive and like all other drugs have their share of side effects like infections.
Is there any role for physiotherapy in ankylosing spondylitis?
Patients must do regular exercises that promote spinal extension and mobility as advised by the doctor and physiotherapist. Activities like aerobics, walking, swimming etc are encouraged
Do patients with ankylosing spondylitis need Surgical treatment?
Total hip replacement is done for those with severe hip arthritis. Spinal surgery is rarely needed to correct excess deformities of the neck or for low trauma fractures.
What are the other problems that are associated with ankylosing spondylitis ?
Uveitis : Inflammation of a part of eye causing redness with or without pain. Eye examination by ophthalmologist as and when suggested by your Rheumatologist is a must for AS patients.
Psoriasis : Any changes in skin, nail and scalp must be reported to your Rheumatologist .in the form of Patches, scaly plaques, discolored nails ,excessive dandruff could be psoriasis which is seen in some patients with AS and vice versa. Psoriasis is managed in conjunction with a dermatologist.
Gastrointestinal symptoms : diarrhea and constipation could be due to intestinal inflammation which need further evaluation by Rheumatologist in conjunction with gastroenterologist.
Osteoporosis : Long standing AS and those with fused spine are at risk for developing osteoporosis which needs evaluation by the Rheumatologist. You may need to take calcium and vitamin D supplements and anti-osteoporotic as prescribed by Rheumatologist
I have AS. I have heard that it runs in families. Should I plan a family?
If you are HLA B 27 positive & your child inherits the gene, there is only 5- 20% chance that he/ she will develop AS. If you are HLA B 27 negative, then the chance of your child developing AS is even lower. Hence you AS should not deter you from starting a family.
Should I get my child’s HLA B 27 test done?
As pointed earlier HLA B 27 alone does not necessarily mean AS. Even if your child is HLA B 27 positive, the risk of him/ her developing AS is only 5-20%. There are no known preventive strategies known as of now to prevent future development of AS. Hence, getting your child HLA B27 test does not serve any purpose if he/ she has no symptoms of AS.
Is stem cell therapy useful for ankylosing spondylitis?
No. Stem cell therapy for AS is in experimental stages & is currently not approved/ proven to be useful for AS.
Does smoking affect ankylosing spondylitis?
Yes. Smoking has been shown to increase the inflammation of AS & also reduce the responsiveness to therapy.



Who is more prone to get AS?
AS is usually diagnosed in young adults, with a peak age of onset of 20 and 30 years and it is three times more, in males than in females. Studies have shown that individual's risk of developing AS increased 5 to 16 fold if there was a first degree relative (parent, sibling, or child ) with AS. The presence of a gene called HLA-B27 could explain the risk of developing AS.
What causes it?
Though the origin of AS is still unknown, we do know a lot about how it progresses and why it causes spinal stiffening. It is now thought that it involves the body's immune system and that a triggering agent causes the disease and only in people with a genetic or inherited susceptibility.
What happens in AS?
The disease initially begins in the bone at the periphery of the joint and at the site where the ligament is attached to the bone, called as enthesis. The inflammatory cells at the periphery of the bone progressively increase resulting in the weakening of the bone and the body resist the weakening by attempting continuous new bone formation, As the disease process continues the bone may become weaker and weaker. When the inflammation finally burn out the body resond with excessive bone formation in an attempt to repair the damaged bone and in this process this calcification spreads to the ligamentous and even the discs. This finally results in fusion of the adjacent bone also called as bony ankylosis, which is the characteristic feature of the disease as the name suggests.
Symptoms
The most common symptom of AS is chronic low back pain and buttock pains. This back pain has the following characteristic: Begins in early adulthood (age 20 to 30); Gradual onset (rather than sudden onset after an acute injury); lasts longer than three months; worse after rest(for example in the morning); improved with activity; Wakes patients up in the second half of the night ; can cause morning stiffness lasting more than 30 minutes and can cause buttock pain that alternates between the left and right side. In the long term the flexibility of the back mat be reduced due to fusion. Arthritis in other joints may also occur. Enthesitis also causes pain in the elbow, heel and rib etc . Chronic inflammation may cause significant constitutional symptoms in the form low grade fever, fatigue and sometimes weight loss.
AS can affect eyes in 25% of patients. The symptoms of iritis include sudden onset of pain and redness, blurred vision.
Diagnosis
The diagnosis of AS is based upon a combination of a patient's symptoms, physical examination and imaging test. Patient with AS develop characteristic changes in the sacroiliac joints (the joint that connect the tailbone [sacrum] and large pelvic bone [llium]) and spine. These changes can be seen on x-ray images , although the changes take time to develop and may not be apparent until years after symptoms of AS begin. X-ray may be used to diagnose AS in someone whose symptoms, history and physical exam suggest AS. Magnetic resonance imaging (MRI) and computed tomography (CT scanning) are more sensitive than plain X-rays, and may be used if As is suspected but not clearly seen on X-ray .there is no blood test that definitively diagnose ankylosing spondylists, although testing for a gene. HLA-B27, can be helpful in selected groups of patients. Other blood tests, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) may be used in some patients.
Management
Treatment depends on the characteristic and severity of the disease. the sheet anchor in the management is primarily therapeutic exercises, non steroid anti-inflammatory agents, and sometimes disease modifying anti-rheumatic drugs and in those not responding to the above modalities, anti tumor necrosis factor agents has shown promising results in various studies.
Exercise
The exercise consist of posture training, deep breathing, back extension and other stretching movements. The details demonstration of exercises for AS patients is available on the following websites: www.nass.co.uk/exercise.htm safety issues. To avoid developing deformities of the neck, a thin, rather than a thick pillow and prone sleeping may be recommended.
Medications
Nonsteroidal Anti-Inflammatory Drugs(NSAID) are the mainstay of treatment-NSAIDs need to be taken on regular basis and studies have shown that in the long term usage it is known to modify the course of disease also. The therapeutic efficacy of the NSAIDs can be better judged at the recommended dosages and needs at least 2 weeks of regular intake and subsequent long term intake of these medications. The most common side effect of NSAIDs is stomach upset. patient with a current or past history of stomach or small bowel (duodenal) ulcers, bleeding problems, or are on blood thinners (anticoagulants) may require antiulcer agents or other medications such as celecoxib.
Sulfasalazine is a disease – modifying antirheumatic drug, or DMARD, that may be given to slow or stop the progression of AS. This drug provides some relief of arthritis symptoms but has little effect on spinal pain and stiffness. Sulfasalazine can be discontinued if it is not effective after six months of treatment. Side effects of rash, low blood counts can also occur. Patients talking this medicine may need to have blood tests done periodically to monitor blood counts and liver function. Rarely other DMARs like methotrexate may be helpful.
In those patients not responding to NSAIDs and sulfasalazine, theraphy with Anti-tumor necrosis factor agents like infliximab, Etanercept, adalimumab may be considered after careful evaluation by a rheumatologist. These drugs proven to be very efficacious and improvement occurs within a few days to a few weeks of starting the drugs. However, these drugs are probably not very effective in stopping the progression of the disease
Steroids oral steroids is rarely necessary in the treatment of AS and in fact long term use of it may cause increase in bone loss and risk of developing early osteoporosis (weak bones). However steroid ( glucocorticoid injection into the sacroiliac joint and other joints may provide relief in patients who has not therapies.
AS patients are more prone to osteoporosis, hence regular consumption of more calcium and vitaminD can reduce the risk of bone loss. There are other medications that risk of bone loss, such as aledronate, risedronate, zolendronic acid, which can be used in appropriate situations.
Surgery
Total hip replacement, insertion of an artificial hip may be recommended in patients with AS who have severe, persistent hip pain or severely limited mobility due to hip joint arthritis. Spinal surgery-Fusion of the bones in the cervical spine may be recommended for a small number of patients who develop dislocation of these bones and to prevent spinal cord damage. Spinal corrective surgeries like Wedge osteotomy may be required in some patients with severe spinal deformities.
Preventing Complications
As the bones are weak in these patients risk of serious vertebral fractures from slips and falls potentially exists and utmost care to be taken to avoid such mishaps. Sedatives, narcotics and alcohol should be avoided as these agents increases the risk of fall and serious spinal injury. Contact sports and other high impact activities should be avoided. Smoking not only make the disease worse but also places lungs in a mechanically disadvantageous position in already deformed spinal and rib disease due to AS. Hence smoking is absolutely contraindicated in this disease.
Mission
Our efforts are driven by a passionate belief that we can significantly reduce the suffering of Ankylosing Spondylitis. For those yet undiagnosed, it can be reduced by raising awareness & cutting down on the diagnostic delay. For AS warriors, it can be reduced by empowering them to take informed decisions to live a healthy and fulfilling life. We would like to grow as a platform for raising awareness & for mutually beneficial patient- rheumatologist interaction.
Objectives -
- Raise awareness about Ankylosing Spondylitis (AS) among general public.
- Raise awareness about Ankylosing Spondylitis among Family physicians & other specialties.
- Provide the correct information & help AS warriors in taking the right decisions.
- Create a platform for healthy interaction between Rheumatologists, AS warriors & allied healthcare professionals for finding solutions & research.
- Forming local support groups for Ankylosing Spondylitis (AS) warriors
- Work with Rheumatologists, IRA & government bodies towards insurance inclusion & reducing costs of biologics.



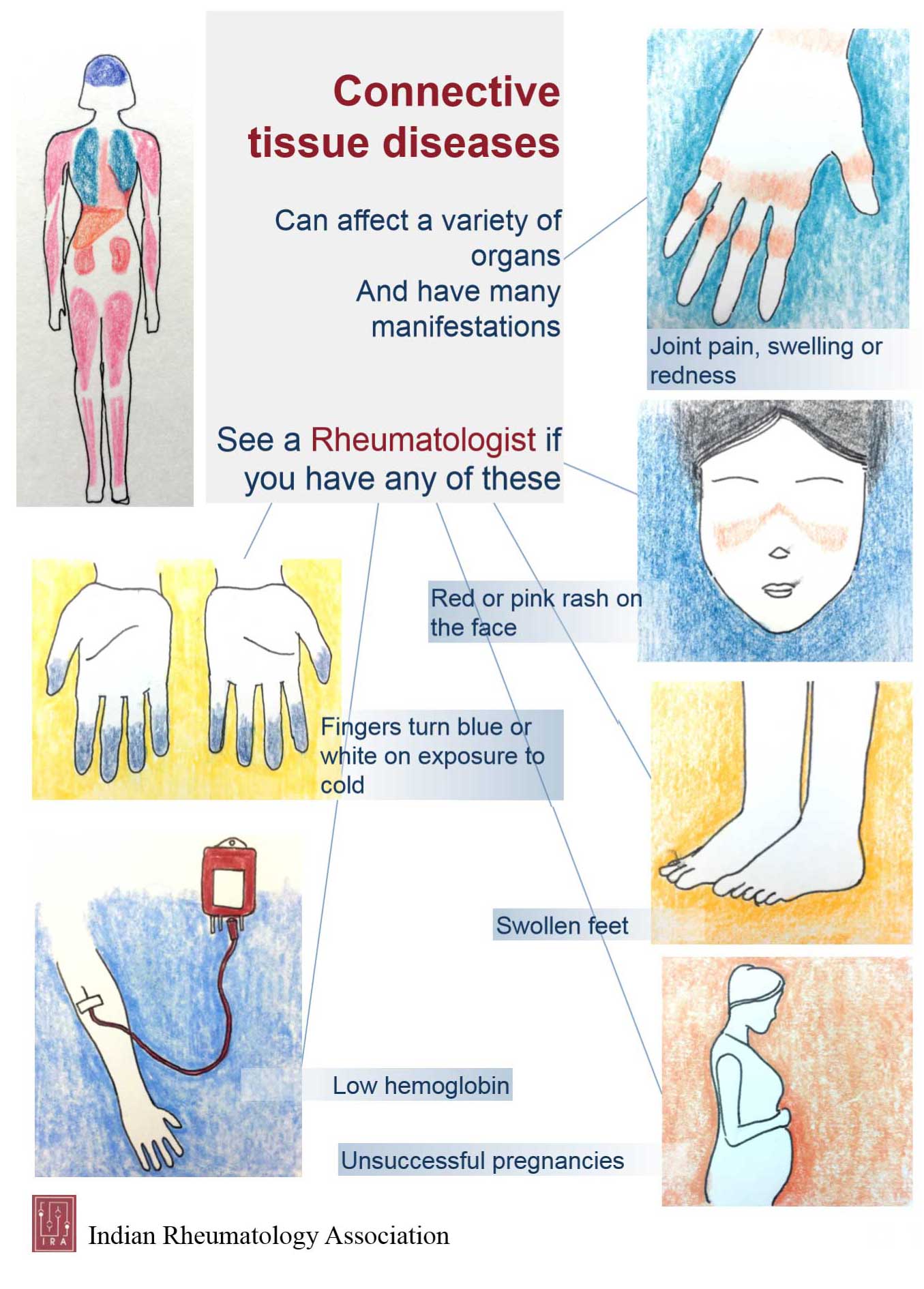
What is Systemic Lupus Erythematosus (SLE/Lupus)?
Systemic lupus erythematosus (SLE/Lupus) is an autoimmune disease. Normally, immune system helps to protect our body from many bad things like infections and cancer. In autoimmune diseases like lupus, one’s own immune system starts attacking its own body. It can occur at any age(mostly 15 to 45 years but can occur in children too). It is seenmore in women than in men.
Please note that we will use the word SLE / Lupus in this article. Both will mean same disease.
What causes SLE / lupus?
The exact cause of SLE is not known. The risk of lupus is associated with what genes are present in one’s body. It has also been found to be associated with environmental factors like sunlight exposure, certain medications, viruses, stress etc. However, in most patients, we don’t find any single gene or environment factor. Mostlikely,it is a combination of many things which causes someone to have SLE.
Who suffers from Lupus?
Lupus is about nine times as common in women as in men.
Lupus is more common in younger women. Lupus also affects children but only rarely. We don't know exactly why this happens.
What are the symptoms of Lupus?
SLE can affect any system or organ of the body. Lupus patients can develop many different types of symptoms.
The most common lupus symptoms are,
- Fatigue or tiredness
- Skin rashes, which get worse on exposure to sunlight. Many patients have a butterfly type of rash on face.
- Joint pain, stiffness more in mornings and joint swelling
- Frequent ulcers (or sores) in mouth or nose
- Hair fall / loss
- Get cold hands and feet, which change color to white or blue, especially when exposed to cold
Lupus patients can also have following symptoms or problems,
- Weight loss
- Frequent fevers without any infections detected
- Headaches and brain problems (like fits or seizures, mood swings, difficulty to think clearly, sudden psychotic or unusual behavior, stroke or paralysis)
- Swelling and puffiness of hands, feet or eyes
- Eye problems – redness, vision problems
- GMuscle weakness
- Recurrent miscarriages, blood clots etc.
- Vomiting, loose stools
- Passing less urine
It is not possible to list all symptoms of lupus here( this may be deleted). Also, having above symptomsdoesn’t itself mean one has lupus. Many of these symptoms like hair fall, fatigue, oral ulcers, swelling etc. are pretty common in people without having lupus. Lupus experts make sure that a patient is not having these symptoms due to other common causes. Most lupus patients will have a combination of many symptoms and experts will do further tests to confirm diagnosis.
Are there any long-term risks in Lupus?
Lupus is a variable and unpredictable condition and can be life threatening for a minority of patients whose vital organs like kidneys, brain, heart, blood etc. are affected. However, with modern treatments and careful monitoring of the condition the disease can be brought under in most patients.
Anything more that I should know?
Keep out of the sun: Use a sun-blocking cream, SPF 25 a greater.
Contraception: You should use contraception pills that contain only progesterone or low-dose estrogen, or consider phyiscal/barrier mehods of contraception. Your treating doctor might help.
Infections: If you have Lupus, and especially if you are on immunosuppressive drugs, then you will more prone to infection. Take sensible precautions and avoid contact with family and friends who are known to have infectious diseases like tuberculosis, chickenpox etc.
Vaccinations: Check with your doctor if you might need vaccinations.
Stress: Stress will make your illness seem worse even if it dosen't affect the course of the disease. Learn how to manage any in your life
Fatigue: Tirendness can be a significant problem. Specific causes of fatigue such as anemia or an underactive thyroid gland can be identified by a blood test and treated.
How is SLE diagnosed ?
When one thinks that a patient has lupus, it is best to get the patient evaluated by experts (Rheumatologist doctors/ other experts). They go into details of symptoms, examine, and after various investigations (blood tests, X ray, urine tests etc.), can make or reject a diagnosis of SLE.
SLE investigations can be very difficult to interpret and no single test can confirm it. Many tests ordered for SLE can come positive in normal people and some tests can be negative even if person has SLE. Hence, only an expert should make a diagnosis of SLE. Once it is confirmed that a patient has SLE, experts might have to do more investigations to find which organs are involved.
How is Lupus managed?
Lupus cannot be cured but it can be controlled. A number of different drugs may be needed depending on which symptoms you experience.
What types of medications are used in treatment of SLE?
Different types of drugs can be used to treat lupus. These are advised according to how severe the disease is and what organs are involved in the patient.The main aim of treatment is to bring lupus disease under control and prevent organ damage.
The drugs used in lupus are to control the overactive immunity which is attacking patient’s own body. They also help to decrease the inflammation in various organs.
- Non-steroidal anti-inflammatory drugs (NSAIDS) : These are drugs like ibuprofen, naproxen etc, especially given if patient has joint pains.
- Medicines like hydroxychloroquine and chloroquine :They were originally discovered to treat malaria, but can help a lot in lupus patients.
- Steroids and other medications (like methotrexate, azathioprine, mycophenolate, cyclophosphamide, rituximab etc.): These help to control or suppress the overactive immune system. Steroids are usually used only at start when disease is moderate to severe.They are very helpful to control disease to give relief and prevent organ damage. Later we use other medications and decrease steroids to maintain the control.
Experts in treating SLE use the drugs given below in best possible way to avoid or minimize the side effects.
I have SLE. Will it affect my chances of getting pregnant and having a good pregnancy outcome?
There are higher chances of problems in pregnancy in SLE females as compared to normal female pregnancies. However, if things are done properly, most lupus patients have healthy babies. Lupus is not a hereditary disease and is not passed to babies as such.
It is important to let your treating doctor know if you want to plan a pregnancy in near future. The expert can guide you and take proper measures to avoid problems in pregnancy. For example, they will advise avoiding pregnancy if your disease is active. However, once your disease is well controlled for at least 6 months, pregnancy can be safely planned under doctor’s advice.
Can one live normally with SLE? Can it be permanently cured ?
SLE can be severe disease. But, most people with SLE can live good lives, provided they showexperts and follow their advice. Continuous research in SLE has made experts learn and improve a lot with regards to SLE treatment over last 20-30 years. They are far better in treating SLE now.
There is still no permanent cure for SLE. Lupus patients will have lupus rest of their lives. It might be mild, moderate or severe. However, as mentioned, we have very good treatment available and the experts provide maximum help to let SLE patients have a good life. SLE patients are likely to live for a long time. In some patients the disease can also become silent without problems for long periods.
Should I try Homeopathy, Ayurveda or even natural therapies for my SLE / lupus ?
Lupus can be a severe disease. Allopathy treatment of SLE has improved a lot with continuous research in last 20 – 30 years and continues to improve with more research. There is no good and thorough evidence that other options (Homeopathy, Ayurveda, natural therapies or Naturopathy) helpto control SLE disease. Many patients trying these therapies develop organ damage which is irreversible. This is because if lupus is not well controlled, it can lead to organ damage. Allopathy can also have side effects, but it is the only form of therapy which has been shown to work without doubt in SLE patients. Allopathy has also been proven to prevent organ damage in SLE patients.
There are many herbs or supplements which can activate the immune systemand cause kidney and liver failure. This can be harmful for lupus patients as their main problem is overactive immunity. If you are planning to take any extra supplements along with your allopathy treatment, please discuss this with your doctor before trying anything new.
What can I do from my end to keep my lupus undercontrolor feel better?
- Have a healthy lifestyle : It can help lupus patients a lot. Eat healthy diet - lots of vegetables, fruits, nuts, dairy products, avoid sugar and refined foods etc. Stay active. Even mild home based exercises, walking and using stairs whenever possible etc are good ways to stay active – It helps Lupus patients to keep muscles and bones strong. Avoid smoking or other addictions.Try to avoid / manage mental and physical stress. One can consider doing relaxation exercises – like meditation or mindfulness etc.
- Avoid excess sun exposure :Sunlight can cause a lupus rash to flare and may even trigger a serious flare of the disease itself. Use a good sunscreen with sun protection factor (SPF) of at least 30 or take doctor’s advice.
- Show an expert in lupus (like a rheumatologist) : Follow their directions
- Get educated about SLE :It is very important for patients to have good information and be educated about their disease, so that they can take better treatment decisions. They shouldask their doctor to provide with patient information material.
- Plan pregnancy : Do let your rheumatologist / doctor know if you want to plan pregnancy. It should be avoided if you have active disease. The doctor can guide with appropriate contraception methods or ways to avoid pregnancy till disease gets controlled.



What is fibromyalgia?
Fibromyalgia (FM) is a disease or sympton complex characterised by widespread pain and profound fatigue.
What causes FM?
The exact cause of FM is not known. It is likely to be multifactorial. Genetic predisposition with disease running families is well recognised. Environmental insults including viral infections, stress (both emotional and physical) and depression in some cases can contribute to the onset of illness. FM can coexist with rheumatic disease like rheumatic arthritis, systemic lupus erythematosus and Sjogren's syndrome.
Who suffers from Lupus?
Lupus is about nine times as common in women as in men.
Lupus is more common in younger women. Lupus also affects children but only rarely. We don't know exactly why this happens.
How common is FM?
It is very common. Upto 3% of the population suffers from it. It is most common around the 4th decade. FM is more common in women but it can occur in men and children too.
How is FM diagnosed?
There is no single diagnostic test for fibromyalgia unlike blood sugar test for the diagnosis of diabetes. The diagnosis is base on the combinations of symptoms, physical examination. Widespread aches and pains affecting both sides of the body are the hallmarks of FM. Neck pain and back pain are the common symptoms. Extreme fatigue, early morning stiffness, non-refreshing and non-restorative sleep, subjective feeling of swelling of limbs and joints, numbness of peripheries are also common. Migraine like headaches, abdominal symptoms like bloating, heart burn, tendency to visit toilet frequently, particularly after food ( irritable bowel syndrome ) and urgency to pass urine frequently (irritable bladder) are other associated symptoms. FM patients also have multiple tender points over the body, which the doctor can identify on examination. So it is the combination of symptoms and the presence of tender points that lead to the diagnosis of FM.
As mentioned earlier, there are no laboratory tests in the diagnosis of FM. Many patients are suspected to have other diseases and are investigated extensively before FM is diagnosed. Your doctor would have ruled our diseases like cancer and arthritis.
What does current research say?
FM is shown now to be a syndrome of low pain threshold and altered pain perception. The volume setting for pain perception is found to be higher in FM patients compared with the normal population. Because of this FM patients would feel more pain compared with non-FM persons for the same amount of stimulus. This process is called central sensitisation, high lighting that the origin of pain is form nervous system rather than in the places where pain in felt. Electrophysiology study of sleep has shown disturbance in sleep apnoea syndrome. Alteration in pain related neurotransmitters, Serotonin and substance P have been demonstraded in cerebrospinal fluid. Abnormalities in sympathetic in cerebrospinal fluid. Abnormalities in sympathetic nervous system, hypothalamo-pituitary adrenal axis, growth hormone secretion have been demonstrated in FM. This might indicate defective mechanisms to fight stress. Some association with depressive illness and other psychiatric illness diseases like chronic fatigue syndrome, non cardiac chest pain, non ulcer dyspepsia, chronic pelvic pain, depression, anxiety and fibromyalgia indicating shared aetiology.
How is FM treated?
Usually FM symptoms are mild and patients mange to lead a normal life in spite of the pain. In some cases, pain can be severe and is comparable with the pain of patients with Rheumatoid Arthritis.
There is no cure. But the symptoms can always be helped. Painkillers like paracetamol and NSAIDs like lbuprofen may be of some help. Unlike the pain of arthritis, the pain of FM does't respond to the above drugs well. It is a different type of pain requiring a different type of medicines. Antidepressant drugs used in doses much lower than what is needed to treat depression are useful is correcting sleep disturbance and in improving pain threshold. Amitriptyline is one such drug. Dothiepin, nortriptyline, Duloxentine, milnacipran are some of the anti depressant drugs found to be useful in managing the symptoms of FM. Anti convulsant drugs ( Anti fits drugs ) like pregablin and gabapentin also help the pain of fibromyalgia.
Cognitive behavioural therapy (CBT) will help patients to take control of his of her illness. This is usually done by trained pain psychologists. Chronic pain leads to in changing the way one think about the illness and encougaes patients to lead a more productive life. Stretching five times a day ) are an important aspect of the therapy.
Walking swimming and cycling are some of the exercise strategies to improve one's stamina and physical conditioning. Pain and fatigue make one de conditioned. Graded increase in the intensity and the duration is essential to overcome post exercise increase in pain. Relaxation techniques like yoga, Tai Chi and low impact dancing and aerobics may help many.
Fibromyalgia is generally treated by a team of pain specialists including rheumatologists, pain consultants, physiotherapists and pain psychologists. More importantly, the patient is an active member of the treatment team.
How to cope up with Fibromyalgia?
- knowing that FM, though a chronic painful disease is not a life threatening or a crippling should reassure you.
- Learn to relax, pace your activities according to pain levels and energy levels.
- Pain does not always mean tissue damage. So don't stop your activities totally.
- Ignore some discomfort, count on functional improvement.
- Be prepared for some bad days and some good days.
- A brief period of rest in between work ( micro-rest) and an afternoon nap can be enterprising.
- Hot water shower and heat in any form will refresh you. A shower in the evening may help you to fresh at dinner time.
- Regular sleep habits will help. Avoid caffeine and cola drinks after 6 PM. Avoid watching movies from the bed. Condition your mind that bed for sleeping. Having the fan on can act as the white noise filter extraneous noises at night.
- Be open with parents, and friends so that they will understand your illness and be more supportive.
- By understanding the nature of the illness, you may be able to avoid unnecessary investigations and harmful therapy.
- Be regular with your exercise and taking the prescribed medicine.
- Discuss with your physician, your doubts and the concerns regarding the disease and the medications.



What is Scleroderma ?
Scleroderma literally means " hard skin," which is a common finding to this group of diseases. It accurs due to the abnormal growth of connective tissue. There are broadly two categories of scleroderma: localized scleroderma ( affects skin and rarely muscles ) and systemic sclerosis ( affects skin and internal organs like heart, lung, intestines etc).
Localized scleroderma generally remains limited and does not progress to the systemic form. Localized scleroderma further can two types; morphea and linear.
Systemic sclerosis affects the skin, muscles, blood vessels and internal organs. It is often divided into diffuse and limited disease. Diffuse systemic sclerosis is a rare disease that can be severe and sometimes life-threatening.
What causes it ?
he exact cause of scleroderma is not known. However, it has been known that body makes too much of collagen ( substance that heals and gives us scars ) that gets deposited in the skin and other body organs, causing the skin to tighten and harden and the organs to dysfunction. Another component is abnormal function of cells in the lining of blood vessels, which leads to Raynaud's phenomenon (pallor, blue fingers or toes) and telangiectasias (red spots). These abnormalities are triggered by abnormal functioning of our own immune cells, some environmental agents of hormones that stimulates cells to produce excess collagen.
Symptoms
Localized Scleroderma
The symptoms of localized scleroderma are isolated ot the skin and underlying tissues. Two types are recognized: morphea and linear scleroderma.
Morphea : These are local patches of hardened skin. Red patches of skin develop white centers with purplish borders. Lesions remain active for weeks to several years. Spontaneous softening that leaves a darkened area of skin often occurs. It may be localized or generalized.
Morphea : These are local patches of hardened skin. Red patches of skin develop white centers with purplish borders. Lesions remain active for weeks to several years. Spontaneous softening that leaves a darkened area of skin often occurs. It may be localized or generalized.
Linear: A single line or band of thickened and discolored skin develops. The line usually runs down and arm or leg, but sometimes it runs down the forehead.
Systemic Sclerosis
This disease affects not only the skin and underlying tissues, but also affects the blood vessels and major organs of the body. Two types of systemic disease are recognized: limited and diffuse.
Limited: In this form, sin thickening is generally limited to the fingers, forearms, legs, face and neck. Raynaud's phenomenon ( blue fingers ) may be present for years before any other symptoms develop. People with this form are less likely than people with diffuse disease to develop severe organ involvement.
Diffuse: In this form, skin thickening may occur anywhere on the body, including the trunk. Only a short interval of time will elapse between the onset of Raynaud's phenomenon and significant organ involvement. Damage typically occurs over the first three to five years, after which most patients enter a stable phase that varies in length. During this phase, your skin will stay about the same and the rate of damage to interval organs slows or stops. After the stable phase is over, your skin will start to soften and more serious damage to internal organs is unlikely to occur.
Depending on the form and severity of the disease, you may experience these different symptoms:
Raynaud's Phenomenon: Cold temperatures or emotional distress cause constriction of blood vessels in hands feet leading to cold extremities and whitish or bluish discoloration of fingers and toes.Once the vessels open back up ( after approximately 10 to 15 minutes), the hands turn red. More than 90% of people with scleroderma have this problem, it is often the first symptom of the disease. Skin ulcers on the fingertips can result from severe Raynaud's phenomenon.
Skin changes: In the early stage skin may appear edematous and it may progressively harden with loss of flexibility. As the disease progresses, the skin will become more thickened, sweat and oil glands will stop functioning, and the skin surface will become very dry and itchy. This stage will persist for one to three years, at which time the skin will begin to soften and thin.
Sclerodactyly: Thickening of the skin of the fingers or toes.
Calcinosis: Calcium deposits can form under the skin or in the muscles. These deposits may cause recurrent ulcers on the overlying skin.
Telangiectasias: Red spots due to dilated capillaries near the surface of the skin can be seen.
Dental disease: If the skin around your mouth tightens, you may not be able to open your mouth very wide.You may also have a dry mouth due to secondary Sjogren;s syndrome. Damage to connective tissues in the mouth can lead to loose teeth. These problems can lead to periodontal disease, tooth loss and difficulty chewing, which can compromise your nutritional status.
Esophageal dysmotility: difficulty in swallowing due to loss of normal movement in the food pipe. It may cause chronic heartburn
Gastrointestinal dysfunction: Dysmotility along the whole gastrointestinal tract can cause reflux, early satiety, bloating, nausea, vomiting, cramping abdominal pain, diarrhea, weight loss and malnutrition.
Lung disease: difficulty in breathing or sense of suffocation are the most common initial symptoms. Similar to skin thickening, lungs can become hard too and loose their elasticity leading to decreased oxygenation. Lung impairment is the leading cause of death in systemic sclerosis. Getting your lung function tested regularly is important for detecting lung disease early.
Kindney disease: sudden rise in blood pressure leading to kidney failure is a dangerous complication. About 80 percent of cases of renal crisis occur within the first four or five years of disease, usually in people with diffuse disease.
Heart disease: Symptoms of heart disease are not seen until late in the course of systemic sclerosis. Symptoms include breathlessness on exertion, palpitations and, less frequently, chest pain.
Is it a contagious disease?
No.
How to confirm the diagnosis?
A diagnosis could take months as the disease unfolds and as the doctor is able to rule out other possible causes of your symptoms. Diagnosis is made clinically by the doctor familiar with the disease. There is no direct blood test that can confirm the diagnosis. Special tests may be ordered to evaluate your lung status ( such as a chest X-ray, pulmonary function tests) and gastrointestinal tract function.
What is the Treatment
No treatment till date has been proven effective in reducing the skin thickening. However, several treatments are very effective at preventing and/ or reducing organ damage from this disease. While treatments are not able to reverse the disease, they may actually prolong life. So treatment dicisions are made on a symptom-by-symptom, organ-by-organ basis.
Raynaud's phenomenon
Dont't smoke. Somoking narrows blood vessels, making Raynaud's worse.
Avoid the cold when possible.
Dress warmly, in layrs. Mitterns are warmer than gloves. Use drugs perscribed by your doctor to improve your circulation ( Calcium channel blockers, angiotensin receptor blockers, ACE inhibitors etc.) Skin sores and ulcers can be treated with nitroglycerin paste or antibiotic cream. Narcotic analgesics may be necessary to treat the pain of these ulcers.
Skin problems
Apply moisturizing creams and lotions frequently, especially after bathing. Apply sunscreen before going outdoors.
Use only warm water in your bath or shower ( hot water is too drying)
Avoid harsh soaps, household cleaners and caustic chemicals. Use rubber gloves if you cannot avoid harsh chemicals.
Itching can be treated with oral antihistamines, topical analgesics and topical corticosteroids
Stiff muscles and joints
Get regular exercise to maintain range of motion and muscle strength.
Use pain killers as prescribed by your doctor.
DO NOT mix up two or more NSAIDs on the same day.
DO NOT take pain killers empty stomach.
See a physiotherapist to stretch contracted joints.
Dental problems
Practice good oral hygience- brush and floss regularly. Use fluoride rinses or prescription toothpastes.
See your dentist regularly.
Keep your mouth moist by taking frequent sips of water, chewing sugarless gum or using saliva substitutes.
Perform facial exercises to help keep your mouth and face flexible.
Gastrointestinal problems
Eat small, frequent meals.
Remian standing or sitting at least one hour after eating.
Avoid late-night meals.
Chew food well.
Proton pump inhibitors, such as omeprazole and lansoprazole, can be taken for heartburn.
Promotility agents may help move food through the gastrointestinal tract.
Antibiotics may relieve diarrhea caused by bacterial overgrowth.
Vitamin supplementation may be needed.
Lung disease
Immunosuppressive drugs such as cyclophosphamide and azathioprine, along with low-dose steroids can be used to treat pulmonary fibrosis.
Vasodilators such as prostacyclin, Bosentan, sildenafil can be used to treat pulmonary hypertension.
Get regular check-ups with your doctor and have lung function tests performed often so that lung disease can be caught early and treated.
Get flu and pneumonia vaccines.
Kidney disease
Measure BP regularly and alert your doctor if it is high. Angiotensin- Converting Enzymes (ACE) inhibitors, including captopril, enalapril and ramipril can effectively manage acute renal crisis by lowering high blood pressure.
Angiotensin II receptor inhibitors may be used to control hypertension when your are not in renal crisis.
Kidney dialysis may be necessary for some patients, atleast temporarily.
Renal transplantation may be necessary if kidney are damaged permanently.
Heart disease
Treatments for heart disease vary according to the way the heart is being affected by systemic sclerosis.
Who is at risk of getting this disease ?
Anyone can get scleroderma at any age. Women are more commonly diagnosed with scleroderma than men. In fact women with the disease outnumber men with it by about four-to-one.
Localized scleroderma is more common in children and young women.
Morphea usually appears between the ages of 20 and 40.
Linear scleroderma usually occurs in children or teenagers.Systemic sclerosis, whether limited or diffuse, typically occurs in people 30 to 50 years of age.
Life expectancy
Localized scleroderma is not life-threatening. Systemic sclerosis patients are at risk of serious complications, kidney disease, Pulmorary Arterial Hypertension (PAH) (high blood pressure in the arteries around the lugs), alveolitis ( inflammation of the lungs), Gastro-intestinal ( GI ) disease and heart damage that can be fatal and adversely affect the quality of life.
Pregnancy
Any female diagnosed with scleroderma needs to check with her physician and obstetrician to discuss possible complications associated with having children. If scleroderma has stabilized, then the physicians are better able to determine if the body can handle pregnancy and childbirth. The genetic risk of transmission of disease to children is negligible.



What is juvenile idiopathic arthritis ( JIA )
JIA is the most common cause of chronic (lasts more than 6 week) arthritis in children. It is of different types depending on the clinical signs and symptoms. In JIA child has joint pain associated with swelling and along with this may have fever, skin rash, lymph node enlargement, backache, red eye, or pain in sole/heel.
Why did my chlid get it?
The exact reason why it occurs is not know. Genetic and environmental factors are thought to play a role but it is not a hereditary disease as only 5% of children have a family history.
What are its common symptoms?
It usually with joint pain associated with swelling, which may involve one to several joints. The child may have malaise, fever fatigue and stiffness in the morning. Some children have high grade fever, skin rash and gland enlargement along with joint pain.
How is it diagnosed?
There is no diagnostic test for JIA. The diagnosis is made by presence of symptoms and signs. Some simple tests are done to excule other diseases and to know the severity of disease.
How to confirm the diagnosis?
A diagnosis could take months as the disease unfolds and as the doctor is able to rule out other possible causes of your symptoms. Diagnosis is made clinically by the doctor familiar with the disease. There is no direct blood test that can confirm the diagnosis. Special tests may be ordered to evaluate your lung status ( such as a chest X-ray, pulmonary function tests) and gastrointestinal tract function.
How is it treated?
To provide immediate pain relief most children are treated with NSAIDs like Naproxen, Ibuprofen etc. In a child with a few joint affected injection of cortisone into the joint is an affective way of controlling disease. Since it is chronic disease a significant proportion of children require disease modifying drugs like Methotrexate. Other drugs used are Salazopyrin, Leflunomide and biologics. Along with medication the child needs balanced diet, splints to prevent contractures, physiotherapy and psychological support.
What dietary precautions should the child take?
No relationship between any special food and JIA has been shown. Potato, pulses etc do not increase joint pains. Balanced diet is must for maintenance of muscle mass, bone strength and adequate hemoglobin in blood. A child who is getting cortisone should avoid food rich in fat and salt.
How long would my child need to take medication?
In oligoarticular variety of JIA the child may need only short term treatment but in majority, long term treatment is required. Drugs are gradually reduced after the disease is controlled and can be stopped once the disease is in remission for 1 year. In some types of JIA treatment is given for long term.
Can the disease be cured?
About one third of children may outgrow the disease and may not have symptoms in adulthood. In the rest the disease follows a relapsing remitting course. In a small fraction the disease may be present throughout.
Can my child go to school?
All effort should be made to help the child attend school and indeed most children with JIA can attend school. Some children may need assistance during disease flares. A discussion with the class teacher often helps.
Will my child be able to do job?
If the disease is managed early and well, most children can study and do a profession. However some children have physical limitation and thus cannot do jobs that involve manual labor. It is good to have a session with your physician when you are making decision regarding career.
What is the long term outcome of this disease?
JIA is a disease with good outcome however 50% of children would have some joint pains during adulthood. Most children can attain good education level and are employable. Good outcome depends on early and effective treatment to control disease activity.
What are its complications?
In systemic variety ( So JIA ) child have fluid around the heart ( pericarditis ) around lungs (pleuritis), myocarditis, marked weight loss rarely a serious condition called macrophage activation syndrome. In other varieties limb length discrepancy, hip joint damage and joint deformities may occur. Uveitis ( inflammation in eye ) can present with redness of eyes, blurring of vision or gradual visual loss. Thus regular eye checkup is needed.
Complications can also be related to therapy like weight gain, short stature, acne related to cortisone. Methotrexate, sulphasalazing and leflunomide may rarely cause lowering of blood counts or liver enzyme abnormalities.
Does it have any effect on puberty?
In most children if the disease is well controlled there is no impact on pubertal growth. In children with SoJiA or polyarticular JIA puberty may be delayed due to persistent disease activity.
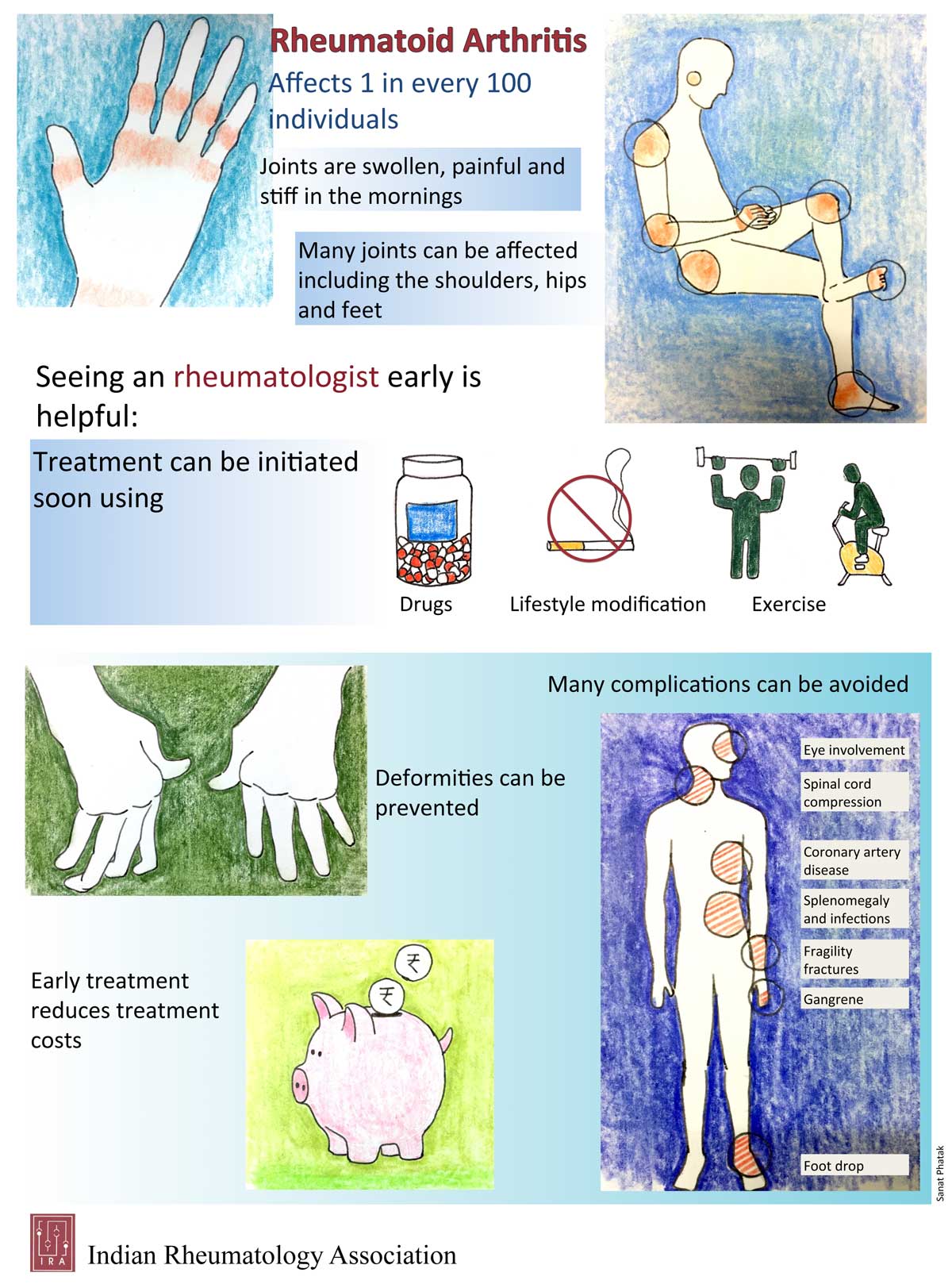
Rheumatoid Arthritis Patient Education
1. What is Rheumatoid Arthritis? What are the common symptoms?
Often as the term arthritis is revealed, views start to pour in from all corners with near and dear ones describing their take on the disease. Often considered as disease of elderly, you are left to ponder why it has happened to you? Where did you go wrong to this disease of “old”. Everyone will feed you with their “general experiences” and adds to dilemma. Remember disease of elderly called osteoarthritis is not same as Rheumatoid Arthritis.
It is important to understand your disease as ignorance here won’t be a bliss. Take command and be the architect of your life. Knowledge about disease helps you allay your fear to some extent
Rheumatoid arthritis is an autoimmune disease which means there are cells in the body which are meant to protect you from foreign invasion like infection, begin to consider your own body as alien for eg your joints. They start attacking your joints. Imagine police who were supposed to keep criminals in check but start attacking civilians.
The disease generally affects small and large joints in a symmetrical fashion and is characterised by pain and swelling in these joints. You may suffer from morning stiffness which can last beyond thirty minutes.
Misfiring of your immune cells may not be limited to joints and you may get other manifestations in theform of long standing cough when lungs are affected or nodules or dryness of mouth or eyes. Knowing your disease well will help you tackle it better because there are so many treatment options available. Important is timely diagnosis and management.
Treatment options are plenty but important is to take medications timely and follow doctor’s advice carefully. We may not cure you but we can help you achieve disease control so that you feel like a healthy individual.
2. What symptoms should alert you?
- Five or more joints involved
- Same joints involved on both sides
- Disease duration more than six weeks
- Early morning stiffness of more 30 minutes or stiffness after a period of rest
- Presence of other symptoms like nodules or dry cough or breathlessness
- Dryness of mouth or eyes ortingling/numbnessor an ulcer
3. How common is the disease?
We don’t have studies spanning the entire nation looking at disease prevalence but remember this is the most prevalent autoimmune arthritis in India and world. It affects females more commonly and can affect any age group from children to adults to old aged individuals. It is seen in one in hundred to one in thousand individuals.
4. What causes RA? Can we prevent it or predict it?
There are multiple reasons which have been explored but none alone can explain this complex disease. Genes, infection and environmental factors all play a role. The triangle below is an overview but remember mere presence of these genetic factors will not give you RA or predict RA. Smoking definitely increases risk, worsens the disease and dilutes the effect of the medications. So it is important you quit smoking before disease makes it difficult for you to even hold a cigarette in your hand.
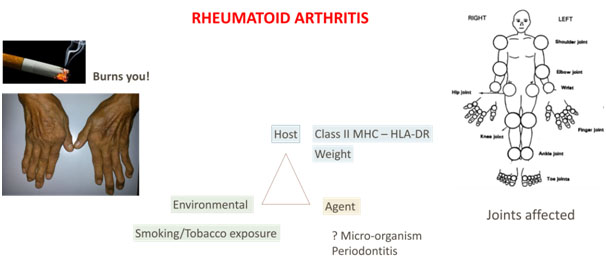
5. What all joints can be affected?
It can affect small and large joints of the body as highlighted in the figure. Small joints include wrist, fingers, toes classically and large joints refer to shoulder, elbow, knee. Hip is less commonly involved. Cervical spine can be affected as well and another joint in the neck called cricoarytenoid can be affected resulting in hoarseness of voice. Occasionally you may notice pain while chewing indicating involvement of temporomandibular joint.
6. Is it familial? Will my kids or siblings suffer the same fate?
There is a genetic component to disease but it does not really predict the chances your relative might get the disease. In fact, even in identical twins, chances of getting RA in other twin, if one has the disease, is only 15-20%. You may question yourself that no one else in your ancestors had this disease then why you?
So it is not necessary that you will get a positive family history or you will transfer the disease to your future generations.
7. Does diet influence disease activity?
Remember, you can have anything you like but if you find particular food item(s) which worsen your joint pain every time you consume, you may stop it. Else there are no dietary restrictions. You can have protein and citrus fruits as much as you like! But remember it is important to manage weight. Ask your doctor what would be an ideal weight for your height.
8. Is there role of stress?
Some people recollect a period of stress or trauma before the advent of these symptoms or may relate to disease flare during periods of stress. It is not clear whether such stressful events are more common or is it a recall bias.
There is a famous quote by Friedrich states he who has a why to live can bear almost any how.
9. What is the natural course of the disease?
It is difficult to predict course in an individual patient but with increasing advancement in Rheumatology, targeted therapy has helped to achieve remission(temporary cure). It is pertinent to start treatment early and adhere to suggestions by the treating doctor. Discuss the treatment options available. Often the treatment is started with methotrexate which works in six to seven out of ten cases. Depending on the drug chosen, you need to give time before they start showing their effect. Discuss with your doctors what to expect. There will be days when disease may flare but remember like in diabetes, there will be times when sugar can go high despite medications, joint pain may increase but can be controlled. Or take another example of hypertension – there can be fluctuations but it can be regulated. Flare of disease means increase in joint pain. Sometimes stress or an infection can flare your disease.
Thus, course can be fluctuating but remember it is often darkest before the dawn. Only in 10-15% of the patients, disease may be resistant. But with increasing awareness, early diagnosis and treatment, large armamentarium of drugs, scenario is improving.
There can be stiffness in the morning or after period of rest but getting back into your daily routine will take away the stiffness. So don’t wait for it to go and then start your day. Do the other way round – start your day and stiffness will go away
10. How to tackle disease flare?
It is important you continue the medications as suggested. Sometimes it can be easily tackled with few days of painkillers. Continue to do you exercises gently. Take warm water bath. Meet your doctor.
11. Is it life threatening?
It can involve multiple other organs other than joints but with good care and compliance for medications, life expectancy is almost same as general population.
12. Myths around RA?
Few important things to note is
- A good healthy lifestyle is always important but it takes multiple factors including genes, environment before the disease manifests.
- It is not contagious
- It is not a disease of “old”
- The drugs, being immunosuppressive, can have side effectsbut remember disease is more disabling. Your doctor will always monitor your side effects and analyse blood tests to monitor same.
- Often you would be told or a doubt may come to your mind – “Will my body get used to of drugs or will I be dependent on them of life?” Yes, but is it not better than being dependent on others? Take command of your life
- Diet has already been discussed –You might be left with only few items to eat if you follow everyone’s advice! Eat as much protein as you like.
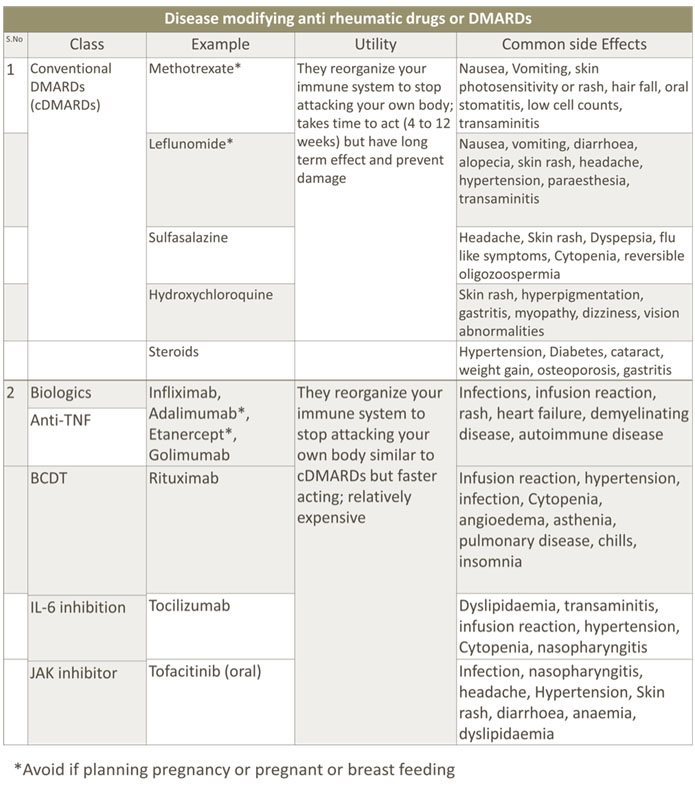
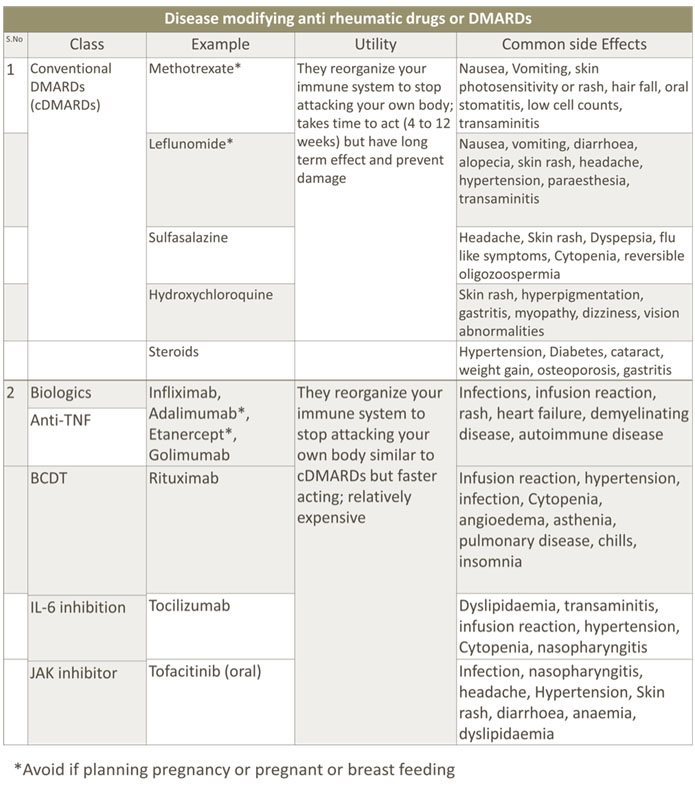
13. What are the medications available and their side effects?
There is a long list of medications available as highlighted in following table along with their side effects profile. You should be aware but not scared of adverse events as it is important to have knowledge about drugs that you might be taking. This will help you understand and adopt them better. Often it is the wrong dose or a drug interaction that does more harm. So a doctor will do your baseline tests before deciding any one of these medications for you and will follow you up with relevant tests routinely to monitor the side effects. So it is important that you spend time with your treating doctor to understand more about them.
14. How long do I need to take medications?
This is another difficult question and there is no straight to answer. Generally, it is lifelong like any diabetes or hypertension. But with early diagnosis, treatment and after a period of sustained remission, it is possible to come down to minimum number of drugs(s).
15. What is remission or low disease activity?
When a doctor uses the term remission or low disease activity, what he or she tends to convey is that your disease is under control with no or minimal pain or swelling in the joint and normal blood reports. He uses certain disease activity indices besides his own experience to decide how active the disease is.
16. Do Ayurveda or naturopathy or homeopathy work?
It is good to discuss with your doctor and inform him if you are taking complementary medications so that drug interactions can be kept in mind. Discuss your experience with the doctor or involve him in taking a shared decision.
17. What is the importance of physiotherapy?
Entire world is realising the importance of yoga and physiotherapy in general. It boosts your immune system, unnerves and relaxes it. In fact, it forms the most important part of your treatment. It is free of cost but needs lot of discipline as we often neglect this mode of treatment. Yoga, aerobics, deep breathing exercise are all very important. Remember it is not just medications alone which will do wonders for you. They are like oil to your body which is a machine! But a machine would rust even if oil is added unless used well!
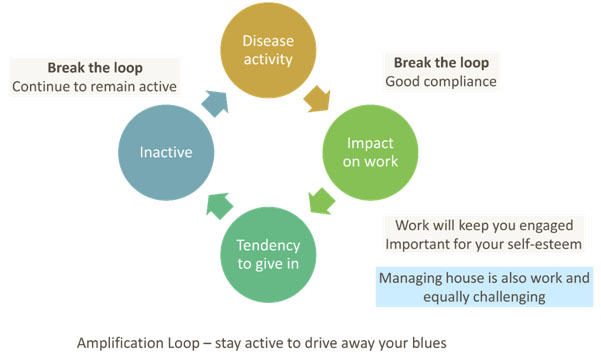
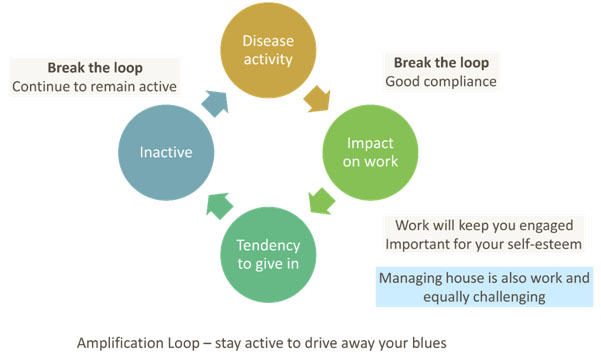
18. Can it affect my work?
Yes,there can be effect on your productivity and efficiency and hence affecting your work. Often the disease activity seems to be controlling the same which is quite obvious. There are two ways to combat it – follow your doctor’s suggestions and continue working as much as possible as keeping yourself active ultimately helps.
Meet an occupational therapist who can help you with your work and activities that you do. They will help you adapt and find ways to make you feel productive.
19. How to maintain energy?
Mix up your day with intermittent breaks for rest, exercise as it helps you to distribute your energy. You may feel tired and fatigued and stiff after periods of inactivity but remember the stiffness is transient and it goes away with activity. Lower your targets and gradually upscale them as you achieve them.
20. Should I share or not share?
This is a personal decision. Don’t let the physical nature of the disease affect you mentally. Stay strong, share if you want, as discussion helps.
21. Is there a cure?
Recent studies are toying with the idea of “cure”. But currently there is no cure but remission or low disease activity with available drugs are achievable. What is most important is timely diagnosis and management.
22. How long will the disease last?
This is another important question which will trouble you more at the onset but sooner or later you will get adapted. Disease tends to last long and the thought can be frustrating but with good compliance and healthy life style, you can lead a constructive life.
23. Does it cause fatigue or low mood?
Yes, it can cause both. Any long standing disease can make you feel so. Inflammation, chronicity of the disease, medications are some of the factors that can make you feel drenched. But with good disease control and exercise, this can be conquered. Often disease affects the decision taking abilities, more out of apprehension, than disease activity per se.
Channelize your energy well by focussing on things in your hand – adherence, exercise and work. Do not burden your joints with lot of backpack. Remember your goal and family and suddenly you will feel all charged up. Set a target. Socialize, mix up with your friends and family. Feel independent. Keep in mind, arthritis is not your identity, your work, your role in society is your identity.
24. What are other complications I should be aware about?
As discussed briefly, RA can affect other organs in the body but can be picked up and treated. Discuss your symptoms with your doctor. Remember to check your blood pressure, sugar and cholesterol as long standing disease can affect your general health. With good disease control and monitoring, these can be prevented or very well taken care of.
25. Can it affect Pregnancy or can I get pregnant?
Yes, you can get pregnant but discuss your medications with doctor. Drugs like methotrexate, Leflunomide and pain killers in third trimester are contra-indicated. Ideally let your disease go into remission or attain a low disease activity status for six months before you conceive. Monitor fetalgrowth, take your medication as advised.
26. How can I contribute?
Remember a doctor learns from a patient more than what he learns from a book. He uses this experience to treat every new patient in a better way. World is moving towards personalised medicine. Therefore, exploring and comprehending the disease is important. His responsibility is to treat you and in an appropriate research setting, he needs to improve the care. You can help by participating in such studies after understanding the impact of such studies. This may not help you immediately but your contribution will definitely help in scientific progress. “We are because you are, and since you are, I am”
What is important is need for constant education/discussion with your doctor and need for re-enforcement as chronicity is double edged sword! You may be gaining more experience but might give up. Don’t just discuss the joints but share you feel. Be you own architect and design your life around it with available resources. Discuss with us and with fellow patients. Take a proactive role and maintain good quality of life.
Rheumatoid Arthritis Patient Education
1. What is Rheumatoid Arthritis? What are the common symptoms?
Often as the term arthritis is revealed, views start to pour in from all corners with near and dear ones describing their take on the disease. Often considered as disease of elderly, you are left to ponder why it has happened to you? Where did you go wrong to this disease of “old”. Everyone will feed you with their “general experiences” and adds to dilemma. Remember disease of elderly called osteoarthritis is not same as Rheumatoid Arthritis.
It is important to understand your disease as ignorance here won’t be a bliss. Take command and be the architect of your life. Knowledge about disease helps you allay your fear to some extent
Rheumatoid arthritis is an autoimmune disease which means there are cells in the body which are meant to protect you from foreign invasion like infection, begin to consider your own body as alien for eg your joints. They start attacking your joints. Imagine police who were supposed to keep criminals in check but start attacking civilians.
The disease generally affects small and large joints in a symmetrical fashion and is characterised by pain and swelling in these joints. You may suffer from morning stiffness which can last beyond thirty minutes.
Misfiring of your immune cells may not be limited to joints and you may get other manifestations in theform of long standing cough when lungs are affected or nodules or dryness of mouth or eyes. Knowing your disease well will help you tackle it better because there are so many treatment options available. Important is timely diagnosis and management.
Treatment options are plenty but important is to take medications timely and follow doctor’s advice carefully. We may not cure you but we can help you achieve disease control so that you feel like a healthy individual.
2. What symptoms should alert you?
- Five or more joints involved
- Same joints involved on both sides
- Disease duration more than six weeks
- Early morning stiffness of more 30 minutes or stiffness after a period of rest
- Presence of other symptoms like nodules or dry cough or breathlessness
- Dryness of mouth or eyes ortingling/numbnessor an ulcer
3. How common is the disease?
We don’t have studies spanning the entire nation looking at disease prevalence but remember this is the most prevalent autoimmune arthritis in India and world. It affects females more commonly and can affect any age group from children to adults to old aged individuals. It is seen in one in hundred to one in thousand individuals.
4. What causes RA? Can we prevent it or predict it?
There are multiple reasons which have been explored but none alone can explain this complex disease. Genes, infection and environmental factors all play a role. The triangle below is an overview but remember mere presence of these genetic factors will not give you RA or predict RA. Smoking definitely increases risk, worsens the disease and dilutes the effect of the medications. So it is important you quit smoking before disease makes it difficult for you to even hold a cigarette in your hand.
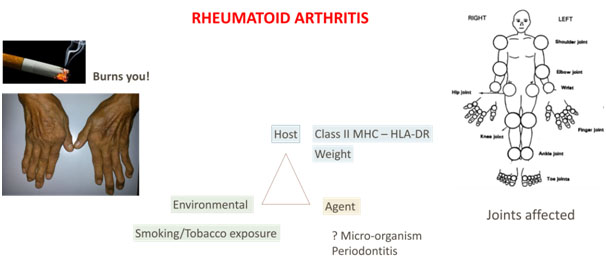
5. What all joints can be affected?
It can affect small and large joints of the body as highlighted in the figure. Small joints include wrist, fingers, toes classically and large joints refer to shoulder, elbow, knee. Hip is less commonly involved. Cervical spine can be affected as well and another joint in the neck called cricoarytenoid can be affected resulting in hoarseness of voice. Occasionally you may notice pain while chewing indicating involvement of temporomandibular joint.
6. Is it familial? Will my kids or siblings suffer the same fate?
There is a genetic component to disease but it does not really predict the chances your relative might get the disease. In fact, even in identical twins, chances of getting RA in other twin, if one has the disease, is only 15-20%. You may question yourself that no one else in your ancestors had this disease then why you?
So it is not necessary that you will get a positive family history or you will transfer the disease to your future generations.
7. Does diet influence disease activity?
Remember, you can have anything you like but if you find particular food item(s) which worsen your joint pain every time you consume, you may stop it. Else there are no dietary restrictions. You can have protein and citrus fruits as much as you like! But remember it is important to manage weight. Ask your doctor what would be an ideal weight for your height.
8. Is there role of stress?
Some people recollect a period of stress or trauma before the advent of these symptoms or may relate to disease flare during periods of stress. It is not clear whether such stressful events are more common or is it a recall bias.
There is a famous quote by Friedrich states he who has a why to live can bear almost any how.
9. What is the natural course of the disease?
It is difficult to predict course in an individual patient but with increasing advancement in Rheumatology, targeted therapy has helped to achieve remission(temporary cure). It is pertinent to start treatment early and adhere to suggestions by the treating doctor. Discuss the treatment options available. Often the treatment is started with methotrexate which works in six to seven out of ten cases. Depending on the drug chosen, you need to give time before they start showing their effect. Discuss with your doctors what to expect. There will be days when disease may flare but remember like in diabetes, there will be times when sugar can go high despite medications, joint pain may increase but can be controlled. Or take another example of hypertension – there can be fluctuations but it can be regulated. Flare of disease means increase in joint pain. Sometimes stress or an infection can flare your disease.
Thus, course can be fluctuating but remember it is often darkest before the dawn. Only in 10-15% of the patients, disease may be resistant. But with increasing awareness, early diagnosis and treatment, large armamentarium of drugs, scenario is improving.
There can be stiffness in the morning or after period of rest but getting back into your daily routine will take away the stiffness. So don’t wait for it to go and then start your day. Do the other way round – start your day and stiffness will go away
10. How to tackle disease flare?
It is important you continue the medications as suggested. Sometimes it can be easily tackled with few days of painkillers. Continue to do you exercises gently. Take warm water bath. Meet your doctor.
11. Is it life threatening?
It can involve multiple other organs other than joints but with good care and compliance for medications, life expectancy is almost same as general population.
12. Myths around RA?
Few important things to note is
- A good healthy lifestyle is always important but it takes multiple factors including genes, environment before the disease manifests.
- It is not contagious
- It is not a disease of “old”
- The drugs, being immunosuppressive, can have side effectsbut remember disease is more disabling. Your doctor will always monitor your side effects and analyse blood tests to monitor same.
- Often you would be told or a doubt may come to your mind – “Will my body get used to of drugs or will I be dependent on them of life?” Yes, but is it not better than being dependent on others? Take command of your life
- Diet has already been discussed –You might be left with only few items to eat if you follow everyone’s advice! Eat as much protein as you like.
13. What are the medications available and their side effects?
There is a long list of medications available as highlighted in following table along with their side effects profile. You should be aware but not scared of adverse events as it is important to have knowledge about drugs that you might be taking. This will help you understand and adopt them better. Often it is the wrong dose or a drug interaction that does more harm. So a doctor will do your baseline tests before deciding any one of these medications for you and will follow you up with relevant tests routinely to monitor the side effects. So it is important that you spend time with your treating doctor to understand more about them.
14. How long do I need to take medications?
This is another difficult question and there is no straight to answer. Generally, it is lifelong like any diabetes or hypertension. But with early diagnosis, treatment and after a period of sustained remission, it is possible to come down to minimum number of drugs(s).
15. What is remission or low disease activity?
When a doctor uses the term remission or low disease activity, what he or she tends to convey is that your disease is under control with no or minimal pain or swelling in the joint and normal blood reports. He uses certain disease activity indices besides his own experience to decide how active the disease is.
16. Do Ayurveda or naturopathy or homeopathy work?
It is good to discuss with your doctor and inform him if you are taking complementary medications so that drug interactions can be kept in mind. Discuss your experience with the doctor or involve him in taking a shared decision.
17. What is the importance of physiotherapy?
Entire world is realising the importance of yoga and physiotherapy in general. It boosts your immune system, unnerves and relaxes it. In fact, it forms the most important part of your treatment. It is free of cost but needs lot of discipline as we often neglect this mode of treatment. Yoga, aerobics, deep breathing exercise are all very important. Remember it is not just medications alone which will do wonders for you. They are like oil to your body which is a machine! But a machine would rust even if oil is added unless used well!
18. Can it affect my work?
Yes,there can be effect on your productivity and efficiency and hence affecting your work. Often the disease activity seems to be controlling the same which is quite obvious. There are two ways to combat it – follow your doctor’s suggestions and continue working as much as possible as keeping yourself active ultimately helps.
Meet an occupational therapist who can help you with your work and activities that you do. They will help you adapt and find ways to make you feel productive.
19. How to maintain energy?
Mix up your day with intermittent breaks for rest, exercise as it helps you to distribute your energy. You may feel tired and fatigued and stiff after periods of inactivity but remember the stiffness is transient and it goes away with activity. Lower your targets and gradually upscale them as you achieve them.
20. Should I share or not share?
This is a personal decision. Don’t let the physical nature of the disease affect you mentally. Stay strong, share if you want, as discussion helps.
21. Is there a cure?
Recent studies are toying with the idea of “cure”. But currently there is no cure but remission or low disease activity with available drugs are achievable. What is most important is timely diagnosis and management.
22. How long will the disease last?
This is another important question which will trouble you more at the onset but sooner or later you will get adapted. Disease tends to last long and the thought can be frustrating but with good compliance and healthy life style, you can lead a constructive life.
23. Does it cause fatigue or low mood?
Yes, it can cause both. Any long standing disease can make you feel so. Inflammation, chronicity of the disease, medications are some of the factors that can make you feel drenched. But with good disease control and exercise, this can be conquered. Often disease affects the decision taking abilities, more out of apprehension, than disease activity per se.
Channelize your energy well by focussing on things in your hand – adherence, exercise and work. Do not burden your joints with lot of backpack. Remember your goal and family and suddenly you will feel all charged up. Set a target. Socialize, mix up with your friends and family. Feel independent. Keep in mind, arthritis is not your identity, your work, your role in society is your identity.
24. What are other complications I should be aware about?
As discussed briefly, RA can affect other organs in the body but can be picked up and treated. Discuss your symptoms with your doctor. Remember to check your blood pressure, sugar and cholesterol as long standing disease can affect your general health. With good disease control and monitoring, these can be prevented or very well taken care of.
25. Can it affect Pregnancy or can I get pregnant?
Yes, you can get pregnant but discuss your medications with doctor. Drugs like methotrexate, Leflunomide and pain killers in third trimester are contra-indicated. Ideally let your disease go into remission or attain a low disease activity status for six months before you conceive. Monitor fetalgrowth, take your medication as advised.
26. How can I contribute?
Remember a doctor learns from a patient more than what he learns from a book. He uses this experience to treat every new patient in a better way. World is moving towards personalised medicine. Therefore, exploring and comprehending the disease is important. His responsibility is to treat you and in an appropriate research setting, he needs to improve the care. You can help by participating in such studies after understanding the impact of such studies. This may not help you immediately but your contribution will definitely help in scientific progress. “We are because you are, and since you are, I am”
What is important is need for constant education/discussion with your doctor and need for re-enforcement as chronicity is double edged sword! You may be gaining more experience but might give up. Don’t just discuss the joints but share you feel. Be you own architect and design your life around it with available resources. Discuss with us and with fellow patients. Take a proactive role and maintain good quality of life.
What is Sjogren’s syndrome?
Sjogren’s syndrome is a disease that affects the glands that make moisture. It causes dryness of mouth and/or eyes. It may also cause joint pains, fatigue and internal organ disease.
Who are likely to develop Sjogren’s syndrome ?
Women are 9 timesmore likely to develop Sjogren’s syndrome than men. Average age of diagnosis is 40 though it can affect all ages and sexes.
What causes Sjogrenssyndrome?
Exact cause is not known. Sjogren’s syndrome is an autoimmune disease in which body’s immune system mistakenly attacks its own organs. In this disease the immune system predominantly attacks organs which are responsible for production of saliva (salivary glands in mouth) and tears (lacrimal glands in eyes).An immune attack on these glands leads to decreased production of saliva and tears leading to dryness of mouth and eyes respectively.
What are the symptoms of Sjogren’s syndrome?
Though dryness of various body organs is the most common symptom in Sjogrens syndrome, as it is a multisystem disease it can present with varied symptoms
- Dry eyes
- Foreign body sensation or grittiness in eyes
- Dry mouth
- Difficulty in swallowing ,talking and chewing
- Dry skin
- Increased tooth caries/decay
- Joint pains
- Excessive Tiredness
- Dry nose
- Dry cough
- Muscle pain / weakness
- Red rashes in the skin
- Thyroid problems
- Numbness and tingling in hands and feet
- Heartburn
- Vaginal dryness
- Painful intercourse
How is Sjogrens syndrome diagnosed ?
This disease is often misdiagnosed or under diagnosed. Rheumatologist is the doctor trained in diagnosing and treating Sjogrens syndrome. After a detailed history, appropriate clinical examination your Rheumatologists will order for some investigations which include blood tests, urine tests and special tests in the eye and mouth. You may be examined by an ophthalmologist (eye doctor), simple tests may be performed on the eye to test the tear flow. Lower Lip biopsy to look for involvement of salivary glands is usually part of diagnostic tests. It is relatively painless minor procedure usually done by dentist. Special immunological tests like Rheumatoid Factor, ANA (Antinuclear Antibody) and ANA profile may also be usually ordered.
Is there a cure for Sjogren’s syndrome ?
Currently there is no cure for Sjogrens syndrome. But early diagnosis and treatment can prevent complications
How is Sjogrens syndrome treated ?
Treatment varies from patient to patient depending on the organ affected.
Dry eyes and mouth :
In addition to artificial tears and saliva, medications like pilocarpine and cevimeline may be prescribed to increase the secretions.
Pain killers and steroids :
Pain killers and steroids may be prescribed as and when needed to treat joint pains. Steroids are also used to treat severe internal organ diseases
Immunosupressives :
Some patients are prescribed immunosupressives like methotrexate, hydroxychloroquine, azathioprine, mycophenolate depending on the internal organ involved.
Life style modifications for dry mouth
- Eat soft, moist foods
- Eat smaller and more frequent meals to stimulate salivary flow
- Avoid salty, acidic, spicy, crunchy tough foods and carbonated drinks which interfere with digestion
- Maintain good oral hygiene by proper brushing, flossing .
- Use alcohol and sugar free mouthwashes
- Regular dental check ups
- Drink plenty of liquids as advised by doctor
- Chew sugar free gum or lozenges or suck sugar free candies to increase saliva flow
- Apply moisturizing gels/vitamin E to dry or sore parts of mouth or tongue for relief
Life style modifications for dry eyes
- Wear sunglasses, shields to prevent moisture evaporation
- Protect eyes from strong air currents that may irritate and aggravate dryness
- Clean the eye lids with clean warm water and mild soap
- Use non preserved artificial tears as advised by doctor
- Avoid regular application of chemicals, commercial products and make up to your eyes
- Ointments and gels can blur the vision, if prescribed must be used in the nights
- Use humidifier at nights to prevent dryness of eyes
Life style modifications for dry skin
- Use warm water instead of hot water for bathing.
- After taking bath, apply Vaseline/moisturizing cream or oil immediately to seal the moisture
- Use sunscreen lotion with minimum SPF 30 on sun exposed areas while going outdoors
Life style modifications for dry nose
- Use Saline sprays, humidifiers to keep the nose moist and crust free
- Avoid air conditioned environment especially in dry mode
What is osteoporosis ?
Osteoporosis is globally the most common metabolic bone disease.Osteo means bone and porous means pore. Osteoporosis means loss of bone density.
What are the types of Osteoporosis? Which type do I have?
Our bones are made up of outer dense cortical bone and inner less dense trabecular bone.Type 1 (early) osteoporosis is characterised by excessive loss of trabecular bone.Type 2 (senile) osteoporosis is characterised by loss of both trabecular and cortical bone which is usually an age related disease.Ask your doctor for the type of osteoporosis.
What are the symptoms of osteoporosis?
Decrease in bone density is usually painless and is diagnosed mostly after patient has sustained a fracture. This is important as In view of lack of symptoms, you may presume you have no osteoporosis even when diagnosed by your physician.
What are the possible complications with osteoporosis?
As long as our bone density is normal,our bones are resilient to low trauma fractures.If bone density decreases there is high risk of fractures even with a minor fall. Ask your doctor what are the chances of fracture?
What are the common sites of osteoporotic fractures?
Common sites include are hip,spine,wrist and ankle.
Why is osteoporosis prevention important ?
- 50% of fractures in the world occur in Asia
- Beyond 50 years one in three females and one in five males sustain fractures due to osteoporosis.
- After sustaining an osteoporotic hip fracture 20-25% die within an year.
- A global survey brought out an interesting fact that number of days spent in hospital is more for osteoporosis and its complications in comparison to the much feared cancers and cardiac ailments.
Who are at risk for osteoporosis ?
The following populations are at risk for developing osteoporosis and need to be aware about the screening and treatment options available.
- Elderly
- Post menopausal women
- Low Body Mass index (BMI)
- Addictions - smokers and chronic alcoholics
- Patients suffering from Rheumatological diseases like Rheumatoid arthritis, Ankylosing spondylitis, Psoriatic arthritis, Lupus and many more
- Use of steroids
- Chronic endocrine diseases like thyroid disorders, diabetes and hyperparathyroidism.
- Malabsorption like celian or Inflammatory Bowel Disease
What are the Screening methods for detection of osteoporosis ?
Dual energy Xrayabosrptiometry DEXA scan is currently the method adopted for measuring bone mineral density.There are two types of DEXA scan - peripheral DEXA which are inaccurate handheld devices used for mass screening purposes and Central DEXA which is an accurate measure of bone mineral density.DEXA scan results are interpreted by your doctor in conjunction with the clinical scenario.
Tips for prevention of osteoporosis
Diet
Its high time we love our bones.Our bones love calcium.Hence the habit of intake of high calcium in diet must start from childhood.Foods rich in calcium are easily available like eggs,milk,curd,cheese,almonds,fish,coconuts,soya,oranges and greens.
Vitamin D
Vitamin D is considered now to be more of a hormone than just a vitamin.It plays a major role in maintaining good bone health.Even a diet rich in calcium becomes useless if our body does not have adequate vitamin D.One and only source of vitamin D that is available in plenty all around us is the sunlight.On exposure to sunlight human skin synthesies vitamin D which is vital for bone health.So daily exposure to sunrays for atleast 20-30 minutes must become a routine habit for all who want their bones to be strong.
Habits
- Avoid smoking
- Restrict coffee or tea to a maximum of two small cups a day ,as excess intake decreases the calcium absorption
- Alcohol >14 units(women) >21 units(men) per week accelerates loss of bone density.
- simple exercises 30 minutes a day for atleast 5 days a week will improve bone strength.
Do’s and Dont’s to prevent falls in elderly
It is of utmost importance to avoid falls in elderly to prevent fractures of hip bone which is the most dangerous fracture beyond 65 years of age in view of the associated mortality and morbidity.
DO'S
- Ensure proper vision
- Good lighting in the room
- Night lamps
- Use crane/crutches/walker/hand railings/modified foot wear according to individuals needs for effective mobilisation
- Use railings for cot to prevent accidental fall from bed
DONTS
- Avoid walking on slippery and polished surfaces
- Avoid walking fast
- Avoid high heels
- Never let mobility restricted people unsupervised or unattended for long periods
Treatment
"Rheumatologist" and endocrinologist are the specialists who usually treat once osteoporosis develops.Therapeutic options for osteoporosis treatment include drugs like oral and intravenous bisphosphonates,hormones like teriparatide and calcitonin,monoclonal antibodies like denosumab.Calcium and Vitamin D supplements according to the severity of the disease is a part of every osteoporosis prescription. These drugs need to strictly taken only under medical supervision.
Those at risk should follow doctors advice on prevention of osteoporosis.
What is osteoarthritis ?
Broadly speaking, arthritis means any joint pain associated with signs of inflammation (swelling, redness, warmth etc). Osteoarthritis (OA) is one of the most commonest arthritis seen in general population. It is a painful condition can that can involve one or more of the joints in the body. It is commonly a disease which occurs with increasing age.
What actually happens in osteoarthritis ?
Often you would hear that there is no or decreased “lubricant” or oil in the joint! Major joints in the body are formed by two end of bones coming together. This end of bones are covered by a cushion, which is known as cartilage. These bone ends along with the cartilage in between forms the joint. This cushion of cartilage is very important in normal functioning of the joint. However in osteoarthritis,there is degeneration and wearing out of the out of this cushion or cartilage. In OA the cartilage thins out along with some other changes in the surrounding bone of the joint and this leads to various problems of osteoarthritis
What are the most common joints involved in osteoarthritis ?
Osteoarthritis can virtually affect any joint. OA most commonly occurs in knees, hips, spine hands,and feet.
What causes osteoarthritis in the joints ?
We are not exactly sure what causes osteoarthritis. However, it is strongly associated with increasing age. Hence age related degeneration of the joint plays a major role. But it is not as simple as that. Many people can develop osteoarthritis at an early age. Many people with osteoarthritis do not have much pain. Many people have osteoarthritis which is much more advanced at an unexpected age. Different patients have variable levels of pain even with same amount of osteoarthritis. Family history is important as well. We arestill trying to understand many of these factors.
What are the risk factors associated with osteoarthritis ?
As mentioned above, we don't totally understand what causes osteoarthritis. However we do know that certain factors play a role in increasing risk of having osteoarthritis.
Age : Advancing age is one of the most commonest risk factors for osteoarthritis. Ingeneral public above 60 years of age, at least 80% have some evidence of osteoarthritis, in at least one of their joints. This may be just seen on X rays and patient may or may not have pain. However as mentioned above, not everyone with the same degree of osteoarthritis will have the same amount of pain.
Gender : For some unknown reasons, females have more chances of osteoarthritis than males. Females also tend to have more pain compared with same degree of osteoarthritis in men.
Obesity and weight : Osteoarthritis occurs more frequently in people who are obese (weight is well above required for that age and height). There is also some evidence that people who reduceweight can decrease the risk of developing osteoarthritis in the future.
Sports and rigorous physical activity : There is evidence that playing excessive injury sports like football, wrestling or repeated kneeling and squatting jobs can increase the risk of osteoarthritis. Having any injury in the ligament in the knee or any other joint can also crease the risk of osteoarthritis in the future . There is good evidence to suggest that routine, non-competitive running or exercises done for personal fitness does not increase the risk of osteoarthritis.
Previous ligament or meniscus injury : Any person who has had a history of injury to their supporting structures in joints like ligaments, meniscus etc at a young age, have higher chances of osteoarthritis in future. This is commonly seen in knee joint ligament and meniscus injuries. Even if one undergoes surgery to repair same, they are still at higher risk for developing osteoarthritis of respective joint in the future.
Family history: Osteoarthritis, particularly, nodal OA, can have remarkable familial predisposition.
Do all patients with age get Osteoarthritis?
No, not all patient get OA and it depends on multiple other factors, some of them have been outlined as above. We don’t have exact figures from India, but OA is more common in women and increases after an age of 50 years and plateaus at 70 years. Western literature shows increasing prevalence over time due to longer life expectancy, obesity and sedentary life style. It is estimated that 10% and 18% men and women are affected respectively.
What are the symptoms associated with osteoarthritis?
Pain :Pain is the most common symptom associated with osteoarthritis. When osteoarthritis starts, the pain can be intermittent and variable. It might be aggravated by certain activities. Often it is more common in late afternoon and evening.The patient can have good days without pain and bad days with pain.
For example : The first symptom of osteoarthritis in the knee is usually having some discomfort or pain while patient is climbing or coming down the stairs.
Site of Pain: Pain more commonly occurs around the joint line except in hip and shoulder when pain can occur away from the joint.
Stiffness or gelling phenomenon : The osteoarthritis patients can have stiffness which is usually aggravated when the patient takes rest in a certain position for more than few minutes. The patients are stiff in the morning but the morning stiffness is usually less than 30 minutes and not very intense like rheumatoid arthritis.
For example : When the patient sits too long with knee osteoarthritis, after getting up, initial few steps are painful. But after walking few steps patient is fine.
Swelling :Some patients with osteoarthritis can have mild to moderate swelling in the joint. This swelling might be soft and compressible due to collection of some fluid in the joint. This can also be hard swelling due to formation of bone spurs (extra new bony protrusions) in the osteoarthritic joint.
Crepitus or crackling sound : In osteoarthritic joint one can have some crackling noise for crackling sound when the joint moves. This is known as crepitus.
For example : Patient with knee joint osteoarthritis can feel crackling or crepitus from their joints, especially when they keep palms over their joint while movements.
In most young – middle aged patients, clicking sounds heard from joints without much pain is normal and one should not start fearing osteoarthritis due to same
How is osteoarthritis diagnosed ?
There is no single test which can diagnose osteoarthritis on its own. Age, weight, family history and pattern of symptoms aid in diagnosis. Other types of inflammatory arthritis, though less common, needs to be ruled out.
Blood tests for osteoarthritis : There is no specific blood test to diagnose OA. Most blood tests done in patients with suspected OA are usually done to rule out other arthritis.
Imaging methods for OA: Sometimes X rays, ultrasound and MRIare helpful in confirming osteoarthritis, but they are not required in most patients. Also, X-ray can be normal in most patients with early OA. Clinical history is most important in early OA. Imaging methods are most useful to identify degree and severity of OA in a particular joint. And it is important to note that pain or clinical findings may not corelate with X-ray findings.
The diagnosis of osteoarthritis is usually made by expert like a Rheumatologist or Orthopedician doctor after collectively taking into account various factors.
How will osteoarthritis progress and affect my daily life ? Will I become permanently disabled ?
Most people will have mild to moderate osteoarthritis with progressive age. In most cases it will lead to mild to moderate pain and usually this pain is intermittent. Most of the osteoarthritis patients can function with good quality of life without doing much interventionsexcept for exercises, assistive devices or being physically active. Howevermany patients will have moderate or progressive osteoarthritis, which can lead to pain and deformities in the future.
In some patients osteoarthritis will disability due to progression. However, there are many non-surgical and surgical treatment options available, even if one has advanced osteoarthritis with disability.
What is treatment for Osteoarthritis ?
General principle of osteoarthritis treatment :
Osteoarthritis is a chronic disease and there is a component of age-related wear and tear (degeneration) of the cartilage in the joint. Because age is a factor, osteoarthritis usually progresses with advancing age. The progress is gradual in most cases and it takes years for patients with early osteoarthritis to develop advanced osteoarthritis and disabilities.
There is no treatment for osteoarthritis which can slow down or stopthe progression of osteoarthritis, except for possible weight control. Most treatment of osteoarthritis is to make the patient symptoms better and to give them a good quality of life.
Osteoarthritis treatment can include a range of options, which can include non-medication based treatment and medication based treatment and surgery. Please understand that every patient is different and every patient with osteoarthritis can have different issues and joints involved. Treatment depends on patient’s exact problems, daily activity demands and their desired expectations from treatment. (Figure 1)
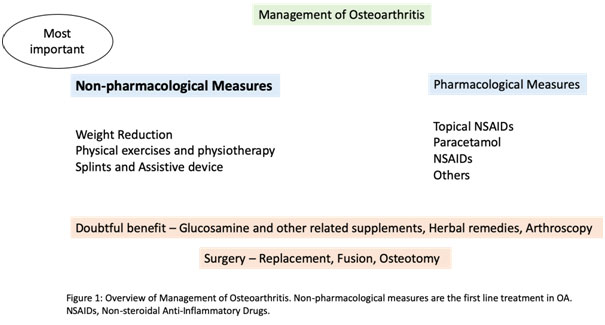
Treatment of osteoarthritis without medication is recommended as a first line of treatment. This line of treatment can be helpful to all patients without any side effects and should be a part of treatment of all OA patients.
Controlling excessive weight or planning weight loss : We have already mentioned that obesity or excessive weight can increase the risk of osteoarthritis. If the patient has already developed osteoarthritis in a particular joint, weight lossmay help to slow down the progression. If Knee or hip joint OA patient loses weight by 10%, there is evidence to suggest that they can have 50% decrease in pain. If one is serious about weight loss, one should strongly consider showing a dietitian who can guide them accordingly with the weight loss program.
Physical exercises and physiotherapy : Exercises are very important part of management of osteoarthritis. They don't improve or stop the progression of the worn-out joint. However they keep to help the surrounding muscles strong and may decrease the pain. So a patient with osteoarthritis who continues to exercise, is more active compared to those who do not exercise. Consider starting exercise gradually and take advice from a trained physiotherapist. They can give specific exercises for affected joint.
Exercise may not give immediate relief and it may take some weeks for exercises to show its benefits. Also, exercises may increase the pain in initial few weeks before they show benefits. The general rule one should follow is any increase in pain after exercise should reach to pre-exercise levels within 24 hours. If that is not the case, one should be more gradual in building up to a desired exercise regimen or take help of a trained physiotherapist to modify the exercises.
Also any form of physical activity in these patients keeps their muscle strong and can be very helpful to help their comorbidities like diabetes, heart disease, hypertension, osteoporosis etc.
Splints and assistive devices : Some patients with osteoarthritis, especially osteoarthritis in the base of the hand can be helped by using hand splints.This splint does not prevent the progression of osteoarthritis in thumb base. However it is helpful inpreventing excess deformity of the thumb base joint. It also helps decreasing the pain at thumb base while movements.
Patients with foot and ankle osteoarthritis may have some specific benefits with some specific insoles. This is generally true if patients have specific issues like flat feet or deviated ankles.
Usually knee braces or stockings are not advisable as they make the muscles surrounding the joints weak (patients muscles are not used and loading is taken by the supportive device). The weak muscles surrounding the joint can further increase the pain and may lead to instability in patient’s movements. However, one might use the supportive devices for intermittent use to provide stability while walking, for short term use before surgery or in cases where surgery is not feasible. Always take advice of a clinical specialist (like a doctor, physiotherapist or occupational therapist).
In patients with advanced osteoarthritis, use of walkers, walking cane or sticks for support etc may be helpful and will prevent falls.
Getting educated and finding some support for patients with osteoarthritis
If one is educated about various aspects of osteoarthritis, they can manage many aspects of their osteoarthritis. This empowers them to deal with this chronic disease more effectively on a daily basis.
Osteoarthritis pain might have a functional component and many people with the same degree of osteoarthritis can have more pain if they don't have a good social support. It is best if such patients can be given some kind of mental or physical support to help with activities at home. Is also helpful if somebody positively encourages to them to do the exercises on a regular basis. It is also very helpful if such patients can join group sessions of people with osteoarthritis. Such groups help them to identify people with similar problems, they can encourage each other to do exercises, provide a listening ear, emotional support etc.
Osteoarthritis treatment with medications/ Pharmacological treatment of osteoarthritis
Most patients with osteoarthritis can be managed with non-pharmacological measures of weight loss, exercise, splints etc. These things should be a part of patient’s management even if any medications are given to them.
Some patients do require medications for management of osteoarthritis. Please understand that there is no medication conclusively proven to halt or slow down the progression of osteoarthritis. Whatever medications we have available right now, are to manage the symptoms of osteoarthritis, so that the patients have better quality of life with less pain and more mobility.
We again re-emphasize that it is very important for the patient to concentrate on exercise and weight loss in most cases, without which the pharmacological interventions maynot have much benefit.
Topical NSAID lotion / gels / therapies for osteoarthritis joints- Topical anti-inflammatory gels / lotions contain drugs called as nonsteroidal anti-inflammatory drugs (NSAIDs).Thesedrugs when applied to the skin over the joint can help in relieving the pain of osteoarthritis. This isespecially true in the hands, knee and other superficial joints. They cannot be usedin relieving pain of hip osteoarthritis as it is a deep joint. Usually topical gels contain very low quantity of NSAID drugs with very low absorption and hence they usually do not have any major side effects. However, in patients with blood pressure, kidney or heart issuesone should discuss safety issues with their doctors.
Nonsteroidal anti-inflammatory drugs (NSAIDs)- Nonsteroidal anti-inflammatory drugs (e.g.: ibuprofen, diclofenac, Naprosyn, indomethacin etc) are commonly known as pain killers by general Indian public. Theynot only help relieve pain but can also help to decrease inflammation (redness, swelling etc). They are very effective drugs in relieving the pain and inflammation associated with osteoarthritis. However, one should always discuss their use with doctor as their consumption in patients with acidity (heartburn), heart, kidney, blood pressure issues etc can be harmful.
Experts might use NSAIDS in short or intermittent courses to help the patients. They will be used in the lowest possible dosesfor the shortest possible duration to avoid side effects.They should not be taken without an expert advice. Some patients might be given low dose of these drugs for prolonged periods. In such cases patients should be educated about side effects and their kidney, liver and other parameters should be regularly checked.
NSAIDS gels (discussed in topical therapies above) have very low doses of these drugs and are absorbed in very little quantities when applied over joints. They are generally much safer to use than NSAID tablets.
Paracetamol - Paracetamol is generally very safe in elderly population of osteoarthritis. The maximum total daily dose of paracetamol is 3 to 4 gram per day. Paracetamol is not as effective as NSAID drugs (discussed above) as it does not have an anti-inflammatory and dramatic pain-relieving effect. However, it is much safer if given for prolonged periods also and can give decent relied to OA patients. In recommended doses it doesn’t tend to affect heart or kidneys.
Paracetamol is commonly used in dose of 500 milligram (mg) for fever 3-4 times per day. However, 500 mg is not usually effective for pain. One should use doses of 650mg-1gm two to three times a day for pain relief in OA. One should be careful with paracetamol doses and should not exceed a dose of 3gram – 4 gram of paracetamol in a day (see table below).
| Paracetamol tablet strength | Maximum tablets which can be safely taken in a day (24hrs) – (do not exceed 4gram in 24 hrs) * |
|---|---|
| 500 mg | 8 tablets |
| 650mg | 6 tablets |
| 1 gram | 4 tablets |
| *Confirm with your doctor |
One should always talk to their doctor before trying to find their maximum possible dose of paracetamol which can be taken safely, and one should take it with regular checking up of liver parameters.
Non NSAID pain relieving drugs: Opioid drugs like tramadol (or tapentadol) tablets or capsules, buprenorphine patches etc are used quite frequently in Indian context. However, there is quite strong evidence that these drugs may cause dependence, can cause a variety of issues including constipation, giddiness, nausea etc. They are generally considered to be unsafe in elderly people and should only be use very sparingly. They are generally not recommended to relieve OA pain routinely.
Neuromodulators for relieving pain: Pain in osteoarthritis and any other disease can be multifactorial. There is some evidence that some patients with OA have over sensitisation of their nerves and this may lead to increase pain. Some experts recommend a trial of low dose neuromodulator drugs like duloxetine, pregabalin, gabapentin etc to give symptomatic relief in OA patients. They might be especially useful in patients with osteoarthritis of spine, especially if there is some compression of nerves. Technically these are not pain relievers, but they possibly work by modulating the pain carried in nerves. Again, these drugs should always be taken under expert guidance.
Joint injections - Glucocorticoid or steroid injections can be useful in certain patients with osteoarthritis. They are especially useful in those with some amount of inflammation in the form of swelling and warmth. They are generally considered to be safe.However, some evidence says that repeated steroid injections in the knee may lead to slightly faster progression of the osteoarthritis. Hence, usually doctors don't give more than three to four injections in a year for a given osteoarthritic joint.
Therapies of uncertain benefits in osteoarthritis
Gel injections in joints:Injection of a certain types of gel in the knee called hyaluronic acid gels are also available(example brand name Hylan,Synvisc,Durolane etc.). Their benefitsareuncertain, don’t last very long and they can be very expensive.
Platelet rich plasma injections in the knee: In this procedure, patients own blood is collected and platelets are separated and injected in the affected joint (mostly knee). It is uncertain if it has any significant benefits. Many patients claim relief but again its uncertain whether they would have got relief anyways from conventional therapies.
Stem cell injections in the OA joints:Off late many centres in India have been propagating use of patients own stem cells to be injected into the OA joint. These are expensive, there is no conclusive benefit, there is no clear-cut guideline or regulatory authority for such kind of procedures. One should at this moment refrain from using these kinds of injections. In most cases utilising the expenses meant these kinds of procedure on replacement surgery is far more beneficial. This is especially true in cases of advanced knee and hip OA.
Glucosamine and other similar supplements: Various tablets / supplements containing glucosamine and chondroitin sulphate are routinely prescribed to or used by patients with osteoarthritis. Many practitioners also prescribe diacerein for patients with osteoarthritis. However, there is no conclusive evidence that any of the above supplements work in relieving the pain of osteoarthritis. There are some good trials which have shown benefit and some good trials which have not shown benefit. There is generally no major harm in using them, but again one should consult their doctor.
Herbal remedies and natural substance supplements for OA: A lot of herbal / natural therapies are there in the market which are claimed to give miraculous relief in osteoarthritis patients. Some patients also claim a lot of relief with these therapies.The list includes many supplements.For example: Turmeric tablets, curcumin tablets, fenugreek tablets, chinese herbal therapies, herbal topical agents, boswellia extract, rose hip extract, Ayurveda therapy tablets or oils etc. These therapies are usually expensive and there is no proven conclusive benefit. However, since they are generally safe the doctors generally do not aggressively discourage the patients from taking these supplements.
One should always be careful of herbal therapies which have the potential to damage liver or kidneys. Many of them claim to have no side effects which can be untrue. Patients should always discuss / disclosetheir herbal therapies they with their respective expert doctors.
Multiple other examples: There are multiple other fancy therapies in unregulated Indian healthcare sector propagated widely to be very effective for osteoarthritis pain. For example: naturopathies, electric stimulation, magnetic therapy, ceragem massages, blood chelation, joint manoeuvring, prolotherapy, cupping etc. They are often expensive, have no proven benefit, might give some placebo effect and may do more harm at times. One should refrain from such therapies or talk to a well-qualified doctor before trying same.
Osteoarthritis surgery
Surgery is usually used as a last resort in osteoarthritis patientsspecially who have advanced osteoarthritis and are not benefited by conservative management. The patients with advanced osteoarthritis have severely worn out cartilage, deformities of the joint and the pain is much more severe.
The various type of surgeries available:
Replacement surgeries:The most common surgery done is knee and hip replacement surgery which can be a partial replacement of a complete replacement.
Replacement is usually done after 55 to 60 years of age as usually replaced joints last for an average of 15 years. Patient’s usually requires a repeat replacement after that. Generally speaking,repeat replacement surgeries are more difficult. As the average Indian age lifespan is around 70-75 years of age, doctors recommend surgery to osteoarthritis patient at around 60 years of age or later. This is so that they are less likely to require another surgery on the same joint in their lifetime.
Fusion surgery: Fusion surgery (medically known as arthrodesis) is recommended in very severe osteoarthritic joint where there is no possibility of a replacement and there is lot of pain.Fusion surgeries are usually done in ankle joint OA where. In fusion surgeries joint margins are fused so that this leads to restriction of joint movement and much lesser pain. However, the movements are obviously restricted after fusion surgery. Such surgeries are more for pain relief at the cost of flexibility of the joint. They can be very helpful in properly selected patients.
Mycophenolate (full name : mycophenolate mofetil) is used to treat variety of rheumatic diseases. This drug is very helpful in controlling the rheumatic diseases. This document is to give information regarding mycophenolate. This will also help patients to address any concerns and understand any precautions regarding taking mycophenolate.
Steroids used for treatment of Rheumatology diseases
Steroids are used to control inflammation rapidly in patients with rheumatoid arthritis and various other rheumatic diseases. This article is meant to give you information on why rheumatologists use steroid tablets or injections. This will also help you understand the various precautions to take or things to understand while taking steroids for rheumatic diseases.
What are steroids used in rheumatology or autoimmune or inflammatory diseases ?
Our body naturally produce some kind of steroids in small amounts. These are necessary to carry out various normal function of the body.
However, we need man-made or external steroids to control the excess inflammation that occurs in rheumatic diseases. Our immune system normally functions to protect us from various infections and internal problems. However, in most rheumatic diseases, the immune system becomes over active. This overactive immune system starts damaging one's own joints or organs. Such diseases are known as autoimmune diseases. Such diseases causes excessive inflammation in various joints or organs. Excess inflammation leads to swelling and can damage to the joints or the organs. Steroids help to control this inflammation rapidly and helps to prevent damage to the joints or the organs.
In which form are steroids used in rheumatology ?
Steroid can be used in either tablet or injection forms.
In the form of tablets.
Prednisolone (commonly known by brand names like Omnacortilor Wysolone) is the most common man-made steroid used in routine medical practice. Sometimes other oral steroids like methylprednisolone or deflazacort are also used.
Steroids can be used in the form of injections in the three ways :
- In very severe rheumatic diseases we might use very high dose of Steroids in the form of an intravenous or iv drip. We call this pulse steroid therapy. This is usually given for 3 to 4 days to control the inflammation very fast if patient has a severe rheumatic disease with severe life or organ threatening issue. We usually use methylprednisolone (succinate) injections for pulse steroids.
- We can also give steroids like methylprednisolone and triamcinolone intramuscularly (in the muscles) in small to moderate doses. These very helpful to control active rheumatic disease or arthritis at the start . This can also be given when the patient has flares or increased disease activity.
- Steroids like methylprednisolone and triamcinolone can also be given locally in the joints as a joint injection.
- This article is mainly meant for patient information on steroid tablets used in rheumatic diseases. The further discussion will be mostly on steroid tablets. The pulse steroid therapy is usually given in hospital setting and the patient can discuss about the same with doctor during that time. Will have a separate article on intra articular or steroid injections given in joints.
Where do we use steroid tablets in rheumatology diseases ?
Steroid tablets are commonly used to treat many rheumatic diseases, especially at the start. They help to bring the disease under control very fast.
They are commonly used in :
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Vasculitis
- Myositis
- Many other inflammatory rheumatic conditions
Depending on the dose given, the diagnosis of patient and severity of disease, steroids can be effective in giving relief in few hours to days.
When should steroid tablets be taken ?
Steroid tablets are usually take once a day in the morning with light breakfast or tea/milk at around 7:00 to 8:00 a.m. It's best to take steroids in the morning as this may possibly cause less side effects. Sometimes rheumatologists might give them on other times of the day.
The dose of steroid tablets will depend on the exact rheumatic disease one has and how active or severe it is. Once the diseases is controlled and other medications are started the steroid is gradually decreased. Now-a-days, in most rheumatic diseases, we are able to decrease and stop steroids after some time. In some cases we might have to continue smaller doses of steroid for maintenance.
We can give this analogy to patients of rheumatic diseases.
Active rheumatic disease is like a hot iron rod/plate. We have tohit the hot iron rod hard with drugs like steroids so that we can get the desired shape. Once we get the desired shape (disease under reasonable control) we can gradually stop or decrease the doses of steroids. Thereafter we try to just maintain the shape (or maintain the disease under control)with disease modifying anti-rheumatic drugs (DMARDs : methotrexate, leflunomide etc)or with low doses of steroids.
I have heard that steroid are verybad for the body and have many side effects. Why should I take steroid tablets ?
In rheumatology we use steroids very judiciously and only when it is absolutely required.
Steroids can be very helpful and a very cost effective method to control the disease very rapidly at the starting phase of the disease. They are very helpful to prevent any damage to joints or any major organs.
For example
- In rheumatoid arthritis we use steroids in very low doses at the start of the disease. This helps to control the disease very fast and gives good pain relief. It has been also shown that giving small doses of steroid in Rheumatoid arthritis can have long lasting good benefits with minimal side effects.
- Systemic lupus erythematosus (SLE) or Lupuscan be an aggressive disease. In this disease the patient can have a major life threatening or organ threatening involvement, eg brain orkidneys etc.We have to use the higher dose of steroids to save life or save the organ. In such patients we might have to carry steroids on a longer-term basis and it might have some side effects. However, these types of patient can have severe problems if we don't you steroids in the right doses.
Today the concept in rheumatology is to you steroids in the lowest possible doses for the lowest possible duration. ARheumatologist will try to decrease your steroid dose if possible in every visit. Also, a rheumatologistcan use some measures or gives advice to prevent or minimise any side effects arising with steroids.
What are the possible risk and side effects with steroid tablets ?
As with any medications, all things can have side effects. You should know about the side effects and can discuss with your doctor about the ways to minimise them.
1) The most common side effect with steroids are
- Weight gain and or increasing appetite
- Weakening of the bones
- Thinning of the skin and easily bruisable skin (mild trauma leads to red patches)
- Indigestion or gastric problems
- Swelling over the face or a round face
- Stretch marks
2) If one is having borderline diabetes or actual diabetes,steroids can also make sugars go higher. It can also increase your blood pressure levels and the doctor should check your sugar and blood pressure at regular intervals while you are on steroids.
3) Steroids can also increase the pressure in eye, specially in patients who have high eye pressure disease known as glaucoma. Use of steroids for more than three to six months in higher doses can also lead to cataract formation.
4) Steroid treatment can also lead to mood changes. People sometimes feel very happy or euphoric on starting steroids and may feel low when the steroids are tapered off. If you are worried please talk to your doctor regarding the same.
5) As we have told before steroids are use do control overactive immunity in patients with autoimmune rheumatic diseases. The steroids can hence suppress the immune system and can increase risk of infections.
What precautions should I take to avoid my risk of infections with steroids ?
ecause there is increased risk of infections while taking steroids,one should take the following precautions to avoid infections.
- Try to avoid coming in contact with people who have active infections which can spread by close contact eg: like flu, tuberculosis etc
- Eat healthy andstay active. That makes you less likely to have infections.
- Keep proper hand hygiene. Always wash your hands regularly, specially before meals and after using washrooms. Try to carry alcohol based hand sanitizer in case you are not able to find a place to wash your hands.
- Try to avoid eating food from sources questionable quality (eg: roadside unhygienic eateries, stale food etc). Even if patient cannot avoid eating outside, they should try to eat things fresh and immediately prepared food. If in doubt try having something hot from the plate as it is likely to be more safe.
One should also inform theirspecialist doctor if they have one of the following while they are taking steroids
- If you have any symptoms suggestive of infection like fever, cough, cold, diarrhoea, or urinary problems, etc
- One should also tell their doctor if they develop chickenpox or shingles or come in contact with somebody having chicken pox.
How to tackle side effects of the steroids ?
- 1) Weight gain - Try to eat healthy foods change your lifestyle and be active
- 2) Weakening of bones : Try to have a good diet with adequate calcium. Doctor might you calcium and vitamin D supplements. In older patients and patients with prior history of fracture we also give some additional tablets to prevent weakening of the bones. Please report any new fracture or any back pain which is sudden in onset (indicating vertebral fracture) to your doctor while you are on steroids.
- 3) Sugars, diabetes and blood pressure : Regularly monitor of sugars and blood pressure. Your physician should be able to adjust diabetes and blood pressure medications.
- 4) Infections : Ways to avoid infection mentioned above
As already mentioned,the doctor will try to decrease the steroid and stop it as soon as possible. They will do this when they feel that it is safe to stop the steroids without causing the damage to the organs. Please take the disease modifying drugs (eg : methotrexate, Leflunomide, mycophenolate, biologicals etc) given by doctor properly. Once they start working we can decrease steroid doses easily.
What is stress doses of Steroids and why do I need to know that ?
Our body produces steroid in a very small amount for normal functioning of the body. This is a very essential thing for the body and our body requires the small amount of natural production of steroids. Our body naturally releases a slightly higher amount of steroids during period of body stress eg : during surgery, during some major infection etc. This helps the body to cope up with the stress of additional disease.
In patients who are receiving man-made or external steroid tablets on a regular basis, the natural body response to produce extra steroids is suppressed. The body in such cases fails to produce a boost of steroids required for the body to cope with the stress. So, in such patients, the doctor might actually have to increase the steroid dose during surgery or infections.
Always inform any doctor you are visiting that you are on steroid tablets along with duration you have been on them. They will decide whether you need extra boost of steroids or not.
Vaccinations while taking steroids
There are many vaccines which can be given to adults besides vaccine given to children. Always discuss any vaccine you are taking with your doctor.
- Patients should not take vaccines with live bacteria while they are on steroids.Live bacteria vaccines are safe in general public. However, because immunity of patients on steroids may be low, live vaccine in them may cause infection and hence should be avoided. Eg of live vaccines : Yellow fever vaccine, chicken pox vaccine, Zostavax shingles vaccine, etc.
- It's usually safe to take vaccines not containing live bacteria in patients on steroids.
Your doctor may advise you some vaccines to decrease the risk of some infections. Usually pneumonia bacteria (one time vaccine) and influenza or flu (every year) vaccines are advised or recommended in rheumatic patients on various medications. However, it will vary for each patient and doctor.
Alcohol
Consuming alcohol in moderation is not a problem while one is on steroid drugs.
Fertility pregnancy and breastfeeding
It is safe to take steroid tablets during pregnancy to control the disease. While one is son steroids one should always discuss pregnancy planning with their doctor. It is best to start planning pregnancy when the primary disease is well controlled and doctor feels it is safe to do so.
Steroid drugs doesn’t affect fertility or one’s chances of getting pregnant.
Very small amount of steroids can pass into breast milk, but it doesn’t cause any harm to baby. It is safe to take steroid tablets while breastfeeding.
Myositis: Expert Speak
What is my disease, myositis, what does it actually mean?
Myositis means inflammation within the muscles. The word inflammation usually includes within it increased temperature, pain, swelling and redness. Your muscles are undergoing these changes.
What are the symptoms of myositis?
The most common symptom of myositis is the weakness of the muscles. This means a loss of strength of the muscles. Movements become difficult to complete often even in the absence of pain.
Can other parts of my body be affected by this disease?
Myositis, which refers to inflammation of muscles, may be associated with inflammation elsewhere in the body also. Commonly affected organs of the body are joints and skin. On occasion, the lungs and heart may be affected. Sometimes this muscle inflammation is the major problem and sometimes it is a part of other diseases like lupus or scleroderma.
How/why did I get this disease? Is it related to pollution, environmental stress, infection or diet?
Each of us carries within all our cells machinery called genes. The genetic makeup of individuals has minor variations that may make a person more easily affected by stresses in the environment than others. These two, genes and the environment combine to form disease. Usually, the body constantly repairs any defect arising out of this combination, but when it cannot contain the bad effects of this combination disease occurs.
Why is my immune system attacking my muscles?
Because your immune system is sensing that there is something different in your muscle cells. So it is seeing them as foreign. The immune cells are trained to sense foreign particles from bacteria, viruses or cancer cells and eliminate them, they try to remove what they think is a foreign particle. This process leads to inflammation which goes on for a long time before the patient can realize the symptoms.
How is the diagnosis confirmed (what all tests do I have to undergo)?
You will need blood tests. These will help to confirm muscle injury. The most common tests performed are blood CPK and LDH levels. The other tests may be ENMG in which a needle will be put in your muscle and the activity of your muscles will be seen on a monitor. The third test is a muscle biopsy. With a small incision, most often in your left thigh, a small piece of your muscle will be taken and examined under the microscope. This is safe and no damage results from the procedure to the muscle. In young children or if there is doubt even after the above tests you may be suggested to undergo an MRI of the muscles. The doctor may decide to do certain special antibody tests for diagnosis if the above tests do not help.
How is myositis treated? What side effects should I be concerned about?
Myositis is treated with steroids. These medicines are very important especially if the muscle weakness is severe. The side effects may include weight gain, acne, change in the shape of the body. Over some time there may be an increase in blood sugar values, a decrease in strength of bones and occasional muscles. When taken over a longer period there may be the formation of cataracts or development of infections. However, the doctor assesses risk-benefit ratio and decides how much steroids to give and in what dose and when to reduce it so that the disease does not come back. To support the steroids and reduce their doses other medicines like methotrexate, mycophenolate mofetil, rituximab may also be chosen.
Can myositis be cured? Will I have to take medications lifelong? Does this disease shorten my lifespan?
Myositis can occasionally be cured. This means that once the treatment is withdrawn it never comes back. More often however the disease may come back at this time. Sometimes it is controlled only partially. Depending on this assessment it is decided how long the medicine has to be continued. The life span is not shortened unless there is the involvement of organs like the lung and heart or very rarely the development of cancer.
What about physical activity and exercise? Will they help or harm me?
After the initial phase when the muscles are weak and sometimes painful, exercise is always encouraged. Exercise in the initial phases may not be possible. Even then it is suggested that someone helps with the movement of muscles. Later as strength improves it is wise to get coached in how to use exercise to strengthen the muscles.
Is there any specific diet that will help my disease or worsen it?
No special diet is recommended or avoided in myositis.
Will my children inherit my disease?
The risk of inheriting myositis is very low.
Any self-care tips?
Keep yourself active. Keep talking to your doctor at frequent intervals about your disease. Eat healthily. Lots of plant-based food, with minimal oil, low sugar, and salt. Exercise regularly.
Any significant new symptom please discuss with your doctor.
Keep yourself active. Keep talking to your doctor at frequent intervals about your disease. Eat healthily. Lots of plant-based food, with minimal oil, low sugar, and salt. Exercise regularly.
Any significant new symptom please discuss with your doctor.
Sjogren Syndrome - Expert Speaks
What is Sjögren's Syndrome?
Sjögren's Syndrome (SS) is a systemic autoimmune disease. An autoimmune disease, as its name suggests is one in which white blood cells that normally protect the body against infection attack different tissues of the body. In Sjögren's Syndrome, the attack is seen against the glands of the mouth and eyes that produce moisture. However, almost any body part can be affected.
Who is likely to have the disease?
Women are more likely to have Sjögren's Syndrome; however, the disease can affect men and children as well.
What are the symptoms of Sjögren's Syndrome?
Patients with SS have varied symptoms. Dryness of eyes and mouth are described as the most common features. Patients may feel the need to drink water repeatedly, drink water to aid swallowing of food and have a gritty or burning sensation in the eyes. However, in India, symptoms of dryness as mentioned above are relatively less common and many patients are oblivious of dryness. Other symptoms suggestive of dryness could also be the complaints. For example, instead of causing an obvious sensation of dryness, lack of moisture in the mouth can result in decay of teeth at an early age, recurrent fungal infection and burning sensation in mouth. Patients can also develop swelling of moisture producing glands. Dryness of vagina is also seen in patients which can cause painful sexual intercourse.

It is very important to remember that Sjögren's Syndrome is not merely a disease of dryness but a systemic disease. By systemic disease, we mean a disease that can affect almost any organ of the body such as the joints, kidney, skin, nerves, brain, lungs etc. And these symptoms can develop before dryness develops. For instance patients can have pain and swelling of the joints, skin rash, weakness and decreased sensation or pins and needle sensation when nerves are affected, cough and breathing difficulty when lungs are affected and so on. Equally important is the fact that many of these symptoms can precede the onset of dryness even by a decade. Many patients also have fibromyalgia (https://indianrheumatology.org/ira-e-newsletter/issue/2020/january/know-your-disease) which is a condition characterized by one or more of the following: aches and pain all over the body, feeling tired easily and sleep disturbances. In patients with long standing disease, 5-10% develops a complication called lymphoma, which is a cancer of white blood cells.

How is Sjögren's Syndrome diagnosed?
Tests for Sjögren's Syndrome should be done in those patients who have dryness or have an organ manifestation suggestive of SS.
There is no single test available for the diagnosis of SS. The diagnosis is made based on a combination of clinical features, tests for evaluating dryness, blood tests and biopsy.
Tests for oral dryness- measures the amount of saliva produced.
Tests for eye dryness- The most commonly done test is caller Schirmer test. This test is done by placing a filter paper inside the lower eyelid and measuring the amount of wetting. You may also be referred to an eye specialist to closely examine the surface of the eye for dryness.
Blood tests include antibodies called anti-SSA (anti-Ro) and anti-SSB (anti-La) antibodies. These may not be positive in all patients. More than 50% of patients also test positive for anti-nuclear antibodies (ANA) and rheumatoid factor. Patients with severe disease have increased protein called globulin in blood.
Biopsy- Biopsy of the glands beneath the lower lip also aids in diagnosis of Sjögren's Syndrome especially if antibodies are negative.
Other useful tests are salivary gland ultrasound and salivary gland nuclear scan (scintigraphy). Sialography involves injecting dye into salivary gland and is less commonly performed.
Why is Sjögren's Syndrome underdiagnosed?
Sjögren's Syndrome is mostly underdiagnosed or misdiagnosed. Some of the reasons may be
- Patients have varied symptoms as described above
- All symptoms may not be present at the same time. Patients may consult different specialists for each of the organ involvement and the patient/different specialists may not be aware of the common connection.
- Many of the systemic features of disease can develop before the appearance of dryness.
- Most Indian patients do not volunteer dryness or may be oblivious to the symptom of dryness.
- Most patients who have antinuclear antibodies (ANA) positive or rheumatoid factor (RF) positive are diagnosed as lupus/rheumatoid arthritis.
Whom should I consult?
Patients with Sjögren's Syndrome are evaluated and treated by rheumatologists as is the case with any autoimmune disease. As patients with SS can have involvement of varied organ systems the concerned specialists are also involved in the care. For instance, those with eye and mouth/dental symptoms should consult an ophthalmologist and dentist regularly.
What are the treatments available?
Treatment depends on the presence of dryness and the degree of involvement of other organ systems. For dryness of mouth, salivary substitutes are available in the form of spray. For dryness of eyes, tear supplements can be used. If no response to the above, drugs that can stimulate secretion of saliva and tears for example, pilocarpine can be used.
In case of systemic involvement, drugs which can modify or suppress the immune system are used based on the severity of disease. The drugs used include hydroxychloroquine, methotrexate, leflunomide, azathioprine, mycophenolate, glucocorticoids, rituximab.
Is there a cure for the disease?
There is no cure for the disease; this need not dishearten you. No cure essentially means that the disease cannot be eradicated totally. However, the disease can be adequately controlled.
Why regular and long term follow up is important?
Regular and long term follow up is important so that complications can be detected well in time and therapy can be tailored to the clinical condition.
Self-care tips
Those who have significant dryness, drink frequent sips of water. Avoid tobacco. Use eye drops as advised. Keep your eye drops and water bottle with you when you are travelling. Inform about the diagnosis of SS to other doctors whom you may be consulting.
Sjögren's Syndrome and pregnancy
Before planning pregnancy, it is extremely important that your disease is under control and that you are not on any medicines that can adversely affect your baby. Most females with SS conceive normally and have healthy babies. However, rarely complications such as abortions, fetal death, fetal heart block or rash in the newborn baby can happen. If there is a history of such complication this needs to be brought to the attention of your rheumatologist and gynaecologist.
This infomration is also available at - https://www.indianrheumatology.org/ira-e-newsletter/issue/2020/july/patients-portal/sjogren-syndrome-expert-speaksFAQs
1. What is meant by antiphospholipid syndrome (APS)?
It is a condition when your immune system mistakenly produces antibodies that attack phospholipids and make your blood much more likely to clot in blood vessels.
2. What are phospholipids and where are they found in our body?
Phospholipids are a type of fat or lipids which occur naturally in all living organisms as the major components of cell membranes including cells lining blood vessels. There are many types of phospholipids.
3. What problems do antiphospholipid antibodies produce in the body?
Antiphospholipid antibodies increase the risk of excessive blood clotting arteries and veins. Sometimes, it also causes low platelet counts.
4. Why do lupus patients get these antiphospholipid antibodies?
Why lupus patients develop antiphospholipid autoantibodies (aPL) is not completely understood. The production of these autoantibodies likely is triggered by an environmental factor, such as an infection occurring in an individual with a genetic susceptibility that makes him or her more susceptible to the disease. 10 to 40% of SLE patients have positive antiphospholipid antibody tests; however, the incidence of clinical APS in them is relatively low(5-10%).
5. How common are these antibodies in the general population?
Antiphospholipid antibodies are found in 1-5% of the normal population. But, incidence of APS is approximately 5 cases per 100,000 persons per year, and the prevalence is approximately 40-50 cases per 100, 000 persons.
6. When would one want to check for these antibodies?
People who develop blood clots especially in young age, repeated miscarriages, low platelet count, or have autoimmune diseases like lupus etc are advised tests for antiphospholipid antibody.
7. What should one watch out for when detected positive for them? Any Do’s and Don’ts?
Birth control pills, smoking and long duration air travel may increase risk of clotting. These are to be avoided. Pain and swelling of the legs and arms, shortness of breath, chest pain, coughing up blood-streaked sputum, numbness, paralysis or weakness of face or limbs, slurred speech are some of the symptoms related to blood clots. You should call your doctor as soon as possible if you develop these symptoms.
8. Are there any preventive measures to be taken during long flights?
Drink plenty of water, discuss with your doctor before planning long travel. Wiggle your toes or keep moving your feet while sitting in the same position during prolonged travel. In addition, compression stockings could be worn in high risk patients.
9. Why do lupus patients get these antiphospholipid antibodies?
Lupus is a disease characterised by the presence of many different types of autoantibodies. Antiphospholipid antibodies are one of them. In fact, they were first discovered in lupus patients.
10. What are their implications during pregnancy and postpartum period in APS patients?
Some of the concerns in antiphospholipid antibodies positive pregnant patients are as follows:
- - Miscarriages, which can occur early i.e. within week ten of gestation (35%) and late in the pregnancy i.e. between week ten of gestation and delivery (17%).
- - Preterm delivery i.e., before week thirty-four of gestation (11%).
- - Intrauterine growth restriction.
- - Blood clots during pregnancy and up to six weeks following the birth of the baby (also referred to as the post-partum period).
- - What are the effects of antiphospholipid antibodies on new born children?
- - Most APS patients give birth to healthy babies
- - Passive transfer of antibodies to the fetus, may result in an increased risk of prematurity, low birth weight, intrauterine growth restriction, thrombocytopenia, and developmental delay.
- - Antiphospholipid antibodies may have an impact on neurodevelopment during fetal life.
- - Although rare, persistence of these antibodies in the neonate may lead to thromboembolism, particularly if there is a concurrent infection and/or inherited thrombophilic disorders.
- - However, the antibodies tend to disappear within the first six months and usually do not result in blood clots in the baby.
- - Neonates born to mothers with antiphospholipid antibody syndrome should have close neurodevelopment follow-up.
11. Do they affect fertility?
Yes, they do.
- Antiphospholipid antibodies interfere with the endometrial decidualization an consequently, with the embryo implantation.
- According to data, the prevalence of aPL in infertile women varies from 4% to 66% and infertility is most commonly linked to presence of Anti b2 GPI antibodies.
12. Don’t anticoagulants used for its treatment cause bleeding, especially heavy menstrual bleeds?
Yes, they do increase the risk of bleeding. A delicate balance needs to be maintained between risk of bleeding and risk of thrombosis. Discuss with the doctor if such issues arise.
Key messages:
- Present treatment for the prevention of the obstetrical complication is quite effective. The majority of the women can have healthy babies.
AND,
- While antiphospholipid syndrome is an autoimmune disease, its diagnosis does not necessarily mean that a patient will develop another autoimmune condition.
This information can also be accessed at https://www.indianrheumatology.org/ira-e-newsletter/issue/2020/october/patients-portal/frequently-asked-questions-aps
* No apparent contraindications for COVID vaccine in AIRD
* Minor adverse events after vaccine reported which are easily managed with minimal supportive therapy
Autoimmune disease, flare and Vaccination
Will my autoimmune disease flare up after vaccination?
A recent study done in New York, published in Annals of Rheumatic diseases, conducted on 1101 participants with rheumatic diseases, showed that around 10 % and 13 % of individuals did have a flare up of their autoimmune rheumatic diseases after the first and second dose of vaccination respectively. However, on a brighter note, majority of the flares (85%) were mild to moderate, with arthritis being the most common flare symptom. The flare lasted for less than 3 weeks in majority of individuals (85%). Based on these interim results, we can say that there is a minimal risk of disease flare or worsening following COVID-19immunization. Regardless, the benefits of immunization are considered to outweigh the potential risks to a very great extent.
Any preference of one vaccine over others?
There is no preference for one vaccine over other whether we talk about efficacy or contra-indication. None of the available vaccines are live vaccines. As far as comparison of efficacy is concerned, there is dearth of data. We will learn more as more people with AIRD get vaccinated.
Co-morbidities, Autoimmune disease and Vaccination
Patients with autoimmune disease and Co-morbidities?
Here co-morbidities would include diseases like diabetes, hypertension, renal disease, stroke, heart attack etc. These co-morbidities put any patient at risk of COVID complication/poorer outcomes. So, it is essential that vaccination should be done at the earliest opportunity. At the same time do not forget to maintain COVID appropriate behaviour strictly.
Optimal timing for COVID-19 vaccination
Another concern is the emerging variants or mutated COVID-19 virus. Infection by one variant may not protect from other emerging variants. But the vaccine is much more likely to give protection against a large majority of prevalent or newly emerging strains/variants. Data shows need for hospitalisation is reduced following vaccine even if you get COVID.
However, current Indian guidelines state that after recent infection, the vaccine should be deferred for 3 months since testing positive. This recommendation is based on the assumption that the antibodies present after a natural infection are protective and may interfere with the vaccine effectiveness.
Unless there is life-threatening infection (means stay in ICU required), there is no need to postpone the vaccine. However, if you have symptoms of COVID-19, you should discuss with your rheumatologist and get tested first.
It should be remembered that is true only for live vaccines and not inactivated or sub-unit vaccines or toxoids (like tetanus toxoid).
DMARDs and Vaccination
Vaccination against COVID19 amongst people living with different autoimmune rheumatic disorders(AIRD) is the need of the hour. Various myths have hampered the vaccination drive amongst the AIRD people. Only 54% of patients with AIRD were willing to taking vaccination as per the recent VAXICOV study. The use of different immunomodulatory drugs has a significant role in the hindrance. It is primarily due to myths related to the fear of drug-vaccine interaction and the misinformation of getting COVID infection following vaccination. As none of the currently available COVID vaccines is a live vaccine, practically there is NO CHANCE of getting INFECTION following COVID vaccination. The only issue is the efficacy of the vaccination may get altered if a particular immunosuppressive medication is continued during the time of vaccination.
Q1. I use Paracetamol or NSAIDs for my pain relief. Can I take vaccine?
Yes, you can take the vaccine as there is no contra-indication or impact of these drugs on Vaccine.
Q2: I am taking oral steroid for my rheumatological problem. Can I take the vaccine? Is it safe for me? Do I need to change my steroid dose?
Vaccination is safe for you, and based on the available data from COVID vaccination and results from other vaccinations in patients with AIRD, neither any dose modification nor any particular schedule required for COVID vaccination in patient on oral steroid.
Q3: I am on Methotrexate (MTX) for my AIRD. Can I take the vaccine? Does the dose of methotrexate affect vaccination timing?
Yes, it would be best to take the vaccine; however, it is preferred to withhold medication one week after each dose of vaccination or two weeks after any single-dose vaccination, provided the disease is under control. Also, there is no difference if you take 15mg/ week or 25mg/ week. It is also essential to know that all these data are borrowed from the impact of MTX on influenza vaccination, and this may change when more data related to COVID vaccination will be available.
Q4: I am on mycophenolate mofetil (MMF) for my interstitial lung disease. Can I take the vaccine? Does the dose of mycophenolate mofetil affect vaccination timing?
Like MTX, the same principle to be followed for MMF. It would be best to hold your medication for one week post each dose of vaccination. It is important to note that stoppage of MMF can lead to disease flare, especially if you are taking that for Lupus nephritis. Better to be in touch with your rheumatologist for decision.
Q5: I am taking Sulfasalazine(SSZ) for my arthritis. Can I take the COVID19 vaccine?
Yes, there is no problem taking the COVID 19 vaccination (any of the COVID vaccines) while you are taking SSZ for arthritis. There is no requirement of any modification of the dose of the drugs or schedule of vaccination. For all practical purposes, for those on hydroxychloroquine, apremilast, IVIG, leflunomide azathioprine, ciclosporin, or tacrolimus, either single or in combination requires no dose or schedule modification.
Q6: I am getting an injection of Cyclophosphamide for my Lupus nephritis. Can I take the COVID vaccine?
Yes, you can take Patients who are on intravenous(IV) cyclophosphamide(CYC), the best vaccination schedule would be at least one week apart from the last/ next dose of IV CYC for better vaccine response.
Q7: I am suffering from ankylosing spondylitis and currently taking injection adalimumab. Can I take the vaccine?
Yes, you can take the vaccine. No special planning is required for COVID 19 vaccination in patients on other TNF inhibitors like infliximab, golimumab, etanercept also.
Q8: I am getting Secukinumab for my psoriatic arthritis. Can I take the vaccine?
Yes, you can take any available COVID vaccines, like those on TNF inhibitors, no special planning required for vaccination.
Q9: I am suffering from Rheumatoid arthritis, and my doctor is planning for the Injection of Rituximab for my disease. When should I take the COVID vaccine?
Rituximab, a CD20 inhibitor, is the only drug used in patients with AIRD has shown a significant effect on vaccine response. Discuss with your Rheumatologist and plan the vaccination schedule to get the maximum benefit. For those at low risk of getting infected, vaccination must be at least four weeks before the next scheduled rituximab dose. On the other hand, if someone has taken vaccination, the Rheumatologist must plan for the next dose of rituximab 2-4 weeks after that, if disease activity permits.
Q10: I am suffering from vasculitis and am on Injection rituximab once every six months. Is it safe to take a vaccine?
Yes, it is safe, and you can take the COVID vaccine. If you have taken the vaccine and your Rheumatologist is planning for injection Rituximab, preferably (discuss with your Rheumatologist, if disease activity permits), wait for 2-4 weeks. There is no harm with Rituximab given earlier, but it will dampen the antibody response, and the vaccine's efficacy may not be optimal. On the other hand, if you have already taken Rituximab and are now planning for vaccination, plan the vaccination schedule 4 weeks before the next rituximab dose, i.e. approximately five months post rituximab.
Q11: I am suffering from Rheumatoid arthritis, and recently my doctor started me on Tofacitinib. Can I take the vaccine?
Yes, you can. However, patients on different Janus kinase(JAK) inhibitors like Tofacitinib or baricitinib withholding drug for one week post-vaccination are preferred to get a desirable vaccine response.
1. I have Lupus with low platelets can I take vaccine?
Yes. Reasons, why this question arises, are a) The route of administration b) Reports of thrombocytopenia and thrombosis in patients following COVISHILED
As far as route is concerned, deep IM injections are generally avoided in those with platelets less than 50,000. Vaccine administration through IM route is not deep enough to result in profuse bleeding and hence can easily be taken. The patient can apply local pressure to prevent hematoma formation if at al.
There are reports of thrombocytopenia but the frequency is very low. The estimated incidence is 1.13 (0.62–1.63) cases per 100,000 doses.
Infact benefits far outweigh the risk. Prevention is always a better strategy as this will allow you to continue most of your lupus medication(s) and hence better control of the disease.
2. Can a lupus patient with neurologic involvement or kidney take vaccine?
Yes, patients with history of neurological disease can take vaccine be it acute transverse myelitis (ATM) or demyelinating neuropathy. Incidence of ATM following vaccine is not known but in the trial only three cases were reported. Of the three cases, only one case was possibly related to Astra-Zeneca Vaccine (Covishield in India). All cases are recovering or have recovered. From India, one case was reported that showed excellent recovery. Having occurred after an administration of >50 million doses, benefits of vaccination seem to outweigh the risk of adverse events. There are reports of Gullian Barre Syndrome (GBS) following COVID19 and COVID Vaccine. GBS following vaccine is very rare when compared to COVID19 including case report(s) following vaccines by Pfizer and Astra-Zeneca. Only one case was reported amongst 37 million doses of Astra-Zeneca in UK. At our institute in SMS, we have seen 12 cases so far and none had an underlying autoimmune disease (unpublished data, Covishield).
Since the risks associated with COVID far outweighs the very rare occurrence of GBS, it is advisable to take vaccination.
Similarly, patients with current or past history of kidney disease or dysfunction can take COVID vaccine. Only concern will be modification of some medication (s) (see Medications section).
No neurological or renal problems are absolute contraindications for any of the vaccines available in India.
I am pregnant in my first trimester- would it be safe to take vaccine?
Currently, we have data from a study done in the USA for the mRNA vaccine (Moderna), which shows expectant mothers mount immune responses similar to the general population. Further, they also found these protective antibodies in the umbilical cord and breast milk, indicating protection to the foetus and newborn as well.
For the benefit offered by the vaccine, it is advisable to take ANY of the COVID-19 vaccines.
Can I have a COVID-19 vaccine if I am breastfeeding?
Yes, there is no harm in taking available COVID-19 vaccines if you are a breastfeeding woman. Though not supported by data, scientifically, no plausible mechanism exists by which any vaccine ingredient could pass to your baby through breast milk. So, it is completely safe to get a vaccination while breastfeeding.
1. Can my child with JIA be vaccinated?
Children with JIA or any autoimmune disease are theoretically at higher risk of getting infection and hospitalised when compared to the general population. However, data from Italy shows children COVID-19 related disease is less frequent and less aggressive. In Italy, 1% of positive cases are under 18 years of age, and no deaths have been recorded before 29 years of age. However, with changing variants, this may change. So it is essential to focus on preventive strategy.
Hence depending on vaccine availability, children with JIA aged 12-17 years or more should be prioritised to receive vaccine and are eligible to receive Pfizer-BioNTech Vaccine. In India, unfortunately, no approved vaccines are yet available. There are ongoing trials on children less than 12 years and once we have the results, we may have more options for this group. Till then ensure proper hand hygiene, social distancing.
Other Vaccines and age group
Pfizer/BioNTech has begun clinical trials to test the safety and efficacy of its vaccine on children ages 6 months to 11 years old.
Moderna has reported that its vaccine showed 96% efficacy in kids ages 12 to 17 in phase II/III clinical trials, and with no major safety concerns. The company is still collecting data and its Phase 2 study in kids ages 6 months to 11 years is ongoing.
2. Can my child with JIA take the vaccine if he is allergic?
Beyond known allergies to vaccine components, there are no known additional contraindications to COVID-19 vaccination for AIIRD patients3. Inform your rheumatologist or pediatrician about allergies.
3. Can my child take other vaccines?
IAP recommends that all routine vaccines should be administered as scheduled without regard to the timing of COVID vaccine. Moreover, there is no evidence to suggest any increased risk of failure or increased side effects if non-COVID vaccines are taken during incubation period of COVID.
If multiple vaccines are administered at a single visit, administer each injection in a different injection site. For adolescents and adults, the deltoid muscle can be used for more than one intramuscular injection.
Others – Number of doses and mixing different types of vaccine
Do we need a third/booster dose?
There are no recommendations as yet though Israel has started giving a booster dose after the second dose. Indian policymakers are yet to come up with such guidelines.
Can I take the second dose with a different vaccine other than the first dose?
Clinical trials in some countries are looking at whether you can have the first dose from one vaccine and a second dose from a different vaccine. There isn't enough data yet to recommend this type of combination.
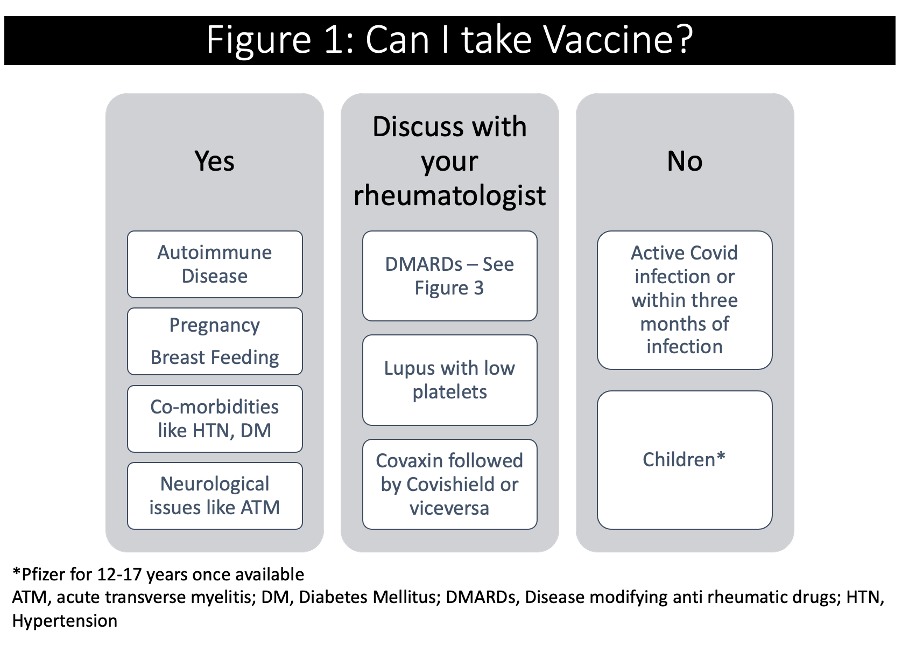
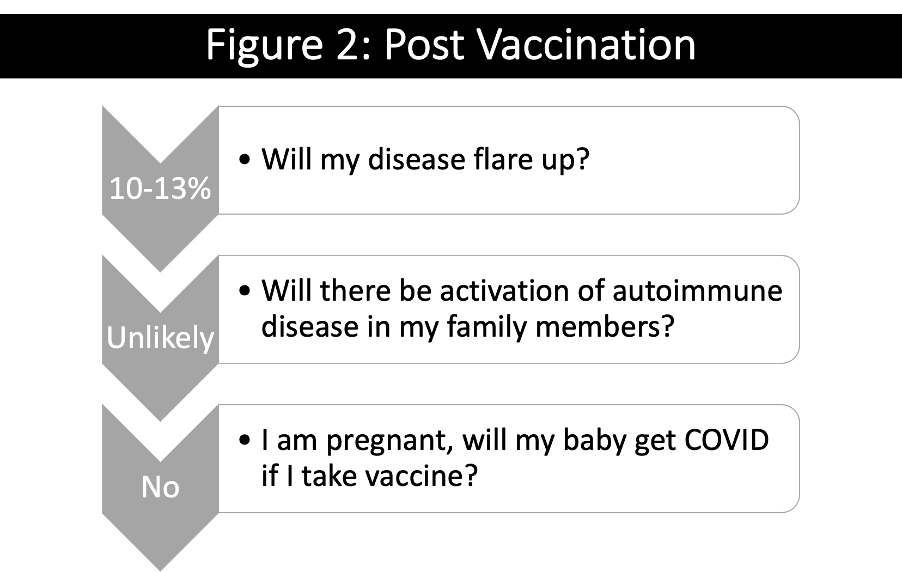
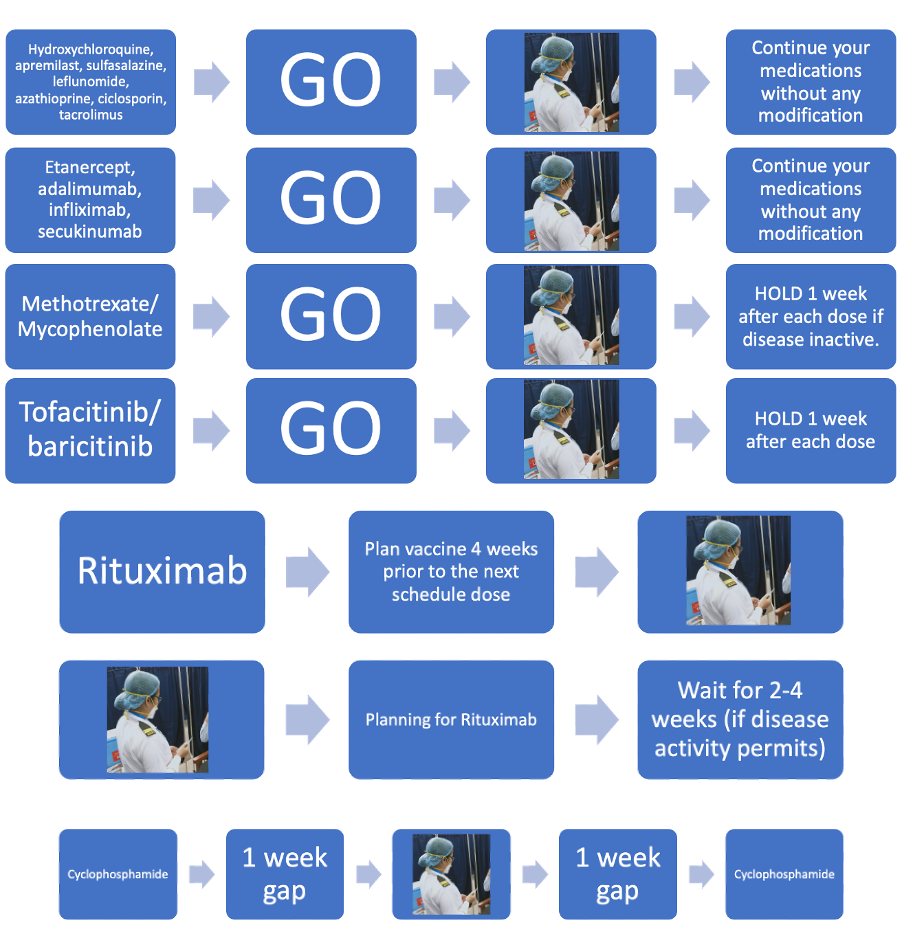
References
Barbhaiya M, Levine JM, Bykerk VP, Jannat-Khah D, Mandl LA. Systemic rheumatic disease flares after SARS-CoV-2 vaccination among rheumatology outpatients in New York City. Ann Rheum Dis. 2021 Jun 22;annrheumdis – 2021–220732.
New Recommendations of NEGVAC accepted by Union Ministry of Health . (2021) from https://pib.gov.in/PressReleasePage.aspx?PRID=1719925
Felten R, Dubois M, Ugarte-Gil MF, Chaudier A, Kawka L, Bergier H, Costecalde C, Pijnenburg L, Fort J, Chatelus E, Sordet C, Javier RM, Gottenberg JE, Sibilia J, Fuentes-Silva Y, Arnaud L. Vaccination against COVID-19: Expectations and concerns of patients with autoimmune and rheumatic diseases. Lancet Rheumatol. 2021 Apr;3(4):e243-e245Simpson CR, Shi T, Vasileiou E, Katikireddi SV, Kerr S, Moore E, et al. First-dose ChAdOx1 and BNT162b2 COVID-19 vaccines and thrombocytopenic, thromboembolic and hemorrhagic events in Scotland. Nat Med. 2021;1–8.
Knoll MD, Wonodi C. Oxford–AstraZeneca COVID-19 vaccine efficacy. The Lancet. 2021;397:72–4
Singh Malhotra H, Gupta P, Prabhu V, Kumar Garg R, Dandu H, Agarwal V. COVID-19 vaccination-associated myelitis. QJM Int J Med [Internet]. 2021 [cited 2021 Jul 7]; Available from: https://doi.org/10.1093/qjmed/hcab069
Vaccines FAQ [Internet]. [cited 2021 Jul 7]. Available from: https://www.idsociety.org/covid-19-real-time-learning-network/vaccines/vaccines-information--faq/
Statement on AstraZeneca Covid-19 vaccine following MHRA update. Available: https://www.gov.uk/government/news/statement-on-astrazeneca-covid-19-vaccine-following-mhra-update [Ref list]
Guillain–Barré Syndrome Associated with SARS-CoV-2 | NEJM. (2021). New England Journal Of Medicine. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMc2009191
Licciardi F, Giani T, Baldini L, Favalli EG, Caporali R, Cimaz R. COVID-19 and what pediatric rheumatologists should know: a review from a highly affected country. Pediatr Rheumatol Online J. 2020;18:35.
COVID-19 FAQS: Juvenile Arthritis [Internet]. [cited 2021 Jul 7]. Available from: https://www.arthritis.org/health-wellness/about-arthritis/related-conditions/other-diseases/covid-19-faqs-juvenile-arthritis
Curtis JR, Johnson SR, Anthony DD, Arasaratnam RJ, Baden LR, Bass AR, et al. American College of Rheumatology Guidance for COVID‐19 Vaccination in Patients With Rheumatic and Musculoskeletal Diseases: Version 2. Arthritis Rheumatol. 2021;art.41877.
Interim Clinical Considerations for Use of COVID-19 Vaccines | CDC [Internet]. 2021 [cited 2021 Jul 5]. Available from: https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html
For more reading, Visit
Centers for Disease Control and Prevention.
Vaccine recommendations and guidelines of the ACIP: COVID-19 vaccine recommendations. March 2021. URL: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19.html.
Centers for Disease Control and Prevention. Vaccines and immunizations: interim clinical considerations for use of mRNA COVID-19 vaccines currently authorized in the United States. March 2021.
URL: https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html.
If someone has received convalescent plasma or monoclonal antibodies (e.g., bamlanivimab, casirivimab, imdevimab) during the COVID-19 infection, they should defer vaccination by 3 months.
Centers for Disease Control and Prevention. Vaccine recommendations and guidelines of the ACIP: COVID-19 vaccine recommendations. March 2021. URL: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19.html.
Coronavirus disease (COVID-19): Vaccines. (2021). https://bit.ly/2Vq9OJU
When should one seek referral to a Pediatric Rheumatologist?
“ It shouldn’t hurt to be a child!” said a young girl with Juvenile Idiopathic arthritis
Are childhood rheumatic diseases rare in India?
There is a common misconception that rheumatic diseases are rare. Juvenile Idiopathic Arthritis (JIA) has an incidence of 1 in 1000 worldwide (and a much higher prevalence) . Henoch Schonlein Purpura and Kawasaki Disease are systemic vasculitides occurring with a reasonable frequency.
More than 50% of rare diseases (diseases that occur in less than 1:2000) occur in children.
The actual problem, however, is not because they are rare, but that they are rarely diagnosed.
What causes rheumatic diseases ?
Rheumatic diseases are related to the immune system. They are due to aberrant or variant responses by the immune system triggered often by an external factor (eg-an infection) in an individual who might have a genetic susceptibility to such response. Occurrence of a rheumatic disease in a child not related to food or any specific factor. It is difficult to predict in advance which child might develop a rheumatic disease as they grow up, but it is important that the disease is identified early and referred to the right experts for management.
Which are the rheumatic diseases that affect children?
-
Arthritis-called as JIA is a spectrum of many different types of joint inflammation. While joint pain can be a symptom of arthritis, the majority of joint pains in children are often benign and transient . The presence of stiffness after rest, especially on waking from sleep, the presence of swelling of the joints, deformities, and limitation of movements are features that suggest a greater possibility of arthritis rather than a benign joint pain.
Some are associated with fever, some with silent inflammation of the eyes, some with inflammation of the spine and so on. All of them can cause long standing disability and deformity if not managed early. Children with uveitis can also develop visual loss, glaucoma, etc. if the right treatment is not given
-
Connective Tissue Diseases- The most common are SLE (Systemic Lupus Erythematous) and Juvenile Dermatomyositis and there are others called Scleroderma, etc. These diseases cause changes in skin, muscle, joints and also in the internal organs . Children often develop prolonged fever with various forms of rashes, bodily discomfort and difficulty with activities of daily living.
-
Systemic Vasculitis- Vasculitis means inflammation of blood vessels and we all know that blood vessels are everywhere in the body. So this group of conditions can also present with manifestations across multiple organ systems .Some conditions like HSP (Henoch Schonlein Purpura) and Kawasaki Disease are seen musch more frequently than conditions like Polyarteritis nodosa and Takayasu arteritis. There is also an Arabian link (the Old Silk Route) in a disease called Behcet’s Disease that presents with frequent painful ulcers in the mouth and genital areas amongst other features.
-
Primary Immune Deficiency disorders are inherited disorders which can sometimes present with rheumatic symptoms and unusual infections.
-
Autoinflammatory disorders- this is a group of conditions, almost always genetic which present as recurrent fever with other typical clinical features. These conditions have become more clear in our understanding in the more recent times and increasing access to genetic testing has improved our ability to confirm diagnoses.
Though we do not have our own incidences of the diseases in India, looking at the population of India and the predominance of young people brings home the sobering reality that there must be a significant prevalence of all these in our country.
All these diseases require early identification and early referral to trained professionals so that appropriate diagnoses can be made and treatment commenced. In all paediatric rheumatic diseases, it is the duration of disease at the point of commencement of specific therapy is what determines the long term outcome . And thus the prevention of disability, death and organ failure .
We are also disadvantaged by an extremely small population of trained health professionals in the field but this is slowly improving.
What are the challenges for children who suffer with these illnesses?
Delayed diagnosis which delays onset of specific therapy.
Almost all of the pediatric rheumatic disease can be controlled very well allowing a normal quality of life even if some require some form of medication lifelong.
Sometimes, workup and investigation can be expensive.
Sometimes, expensive medications may be required for a period to get the disease under control.
Increasing awareness amongst the public, the medical society and all stakeholders is important if we have to get the right treatment to each child.
While every child matters, the charitable help available for children with rheumatic disorders is negligible compared to cancer or heart disease and some of these conditions are as bad as cancer.
Let us move to work together to get these children a better deal. Together, we can make a difference.
FAQs regarding diagnosis and treatment of childhood rheumatic disease
-
What is the nature of treatment of childhood rheumatic disease?
The treatment of childhood rheumatic diseases is with medications, not surgery. These medications can be anti-inflammatory, immunomodulators or immunosuppressants.
-
How long is treatment required?
This is variable. Some diseases like Kawasaki Disease may require medication only for a few weeks to months. Many diseases like Juvenile Idiopathic Arthritis require medications for many years. There are diseases like SLE and some forms of arthritis where medication can be carried on into adulthood and perhaps lifelong .
-
What diet is recommended for a child with rheumatic disease?
There is no specific diet recommendation for a child with rheumatic disease-however there are advantages to encouraging a healthy diet in general with good intake of protein, moderate carbohydrates, high fibre and limiting sugary and salty foods to occasional treats.
For specific situations where the blood pressure is elevated or the child is on high dose steroids there could be further cautions from your doctor.
-
How safe are the medicines? Are there side effects?
All medicines which have an effect can potentially have side-effects too. However, it's important to understand that not everybody gets all the side effects . When the child is on high dose steroids there can be obviously recognisable side effects like weight gain, increased appetite and hair growth etc which are usually reversible upon cessation of the drug. In general, treatment protocols are formulated with the idea of reducing overall steroid exposure as far as possible . In young children very long term intake of daily steroids can also compromise height, hence pediatric rheumatologists are very keen to use “steroid sparing’’ drugs to limit this possibility. Most of the other drugs require regular blood monitoring that the doctor will advise you about and which can pick up drug related side effects earlier than any symptoms. In general, most of the drugs are usually very well tolerated by children with the actual incidence of significant side effects being rare.
-
My child hates Methotrexate – how can I manage this?
This is unfortunately not an uncommon scenario. Especially in Juvenile Idiopathic Arthritis, methotrexate is a cheap and effective medication for many children. However, after the first few months many children develop “ anticipatory nausea” or the feeling of being sick when they see or think of the medication. The strategies employed could be to take anti nausea medications along with the drug that your doctor can prescribe, switching the dose to before bedtime, so they can sleep off the nausea, drinking coffee with and after the drug or consider changing it to the weekly subcutaneous injection form. When the drug is working well for the disease, it would be better to try these strategies including approaching a psychologist who can also give coping strategies rather than trying to stop or changing the drug which is often done only as a last resort.
-
How do I explain this disease to our relatives and neighbours? People are criticising us for allowing our child to take medications for so many years.
This is unfortunately the bane of the Indian social scenario where the complete lack of awareness of these diseases or their management in the public arena leads to such unreliable and dangerous advice. It is important to clear all your doubts with the doctor and be convinced that this treatment is important for your child regardless of what unaware and ignorant peers misinform you.
-
Are there restrictions to future career prospects?
The idea of treating rheumatic diseases early, with appropriate aggression is to allow children to develop normally and attain their full potential as adults. We encourage them to seek any education and career of their choice in the majority of situations. We would like to see the child have the same abilities and aspirations as his peers, the only difference being that he may need to be taking a regular medication.
-
Can my daughter get married in the future?
While many children with rheumatic diseases might go into remission and come off medications before they become adults, there are several conditions like subsets of JIA or SLE where they will need to continue medications as adults. Your pediatric rheumatologist will transition the child to an adult rheumatologist after they move to college and higher educational levels. While marriage and pregnancy are achievable for the majority of these patients, it is important that they discuss these aspects with their rheumatologist. A pregnant lady on treatment for rheumatic disease needs to follow up with both her obstetrician as well her rheumatologist.
-
Can we give them all the vaccinations as per schedule when they are on these medications?
While the majority of vaccines can be given, it's important to discuss with your pediatric rheumatologist who can instruct the general pediatrician as to the timing and type of vaccines to be given to a child on treatment for rheumatic disease.
-
Can we try alternative medicine? My neighbours tell me there are no side effects.
This is a common question. It is important to realise that there are no alternative medicines, only evidence based medicines. Most traditional forms of medicine have not been subjected to scientific scrutiny regarding their outcomes in rheumatic disease or their side effects and hence such recommendations cannot be given at the present time.
-
What lifestyle restrictions should these children have? Can they take part in sports and school activities and other physical or artistic pursuits like martial arts/dancing?
Indeed, yes. Once the active discomfort of their symptoms are reduced, we encourage activity as they feel comfortable. Even during active disease we encourage some movement rather than complete rest. I have patients who excel in sports, dancing and martial arts.
-
Should we tell the school about the diagnosis?
Most definitely, yes. The teachers need to be aware that the child may have some physical difficulties in the initial phase and that their medications do increase their risk of catching infections easily and try to seat them in the classroom mindful of this possibility. They should understand that the child would need occasional days off school for medical appointments and support them to integrate into the classroom rather than stay away from school.
A child who has recovered from Juvenile Dermatomyositis has now trained to become an exponent of a demanding traditional martial art form of Kerala called kalaripayattu. Images uploaded with consent from patient and parents.